The Effect of Ezetimibe in The Treatment of Ebola
Received Date: March 28, 2022 Accepted Date: April 28, 2022 Published Date: April 30, 2022
doi: 10.17303/jvrav.2022.1.103
Citation: Ali Khanifar (2022) The Effect of Ezetimibe in The Treatment of Ebola. J Vir Res Adv Vac 1: 1-9.
Abstract
In this article, we are looking for treatment for Ebolavirus.We will do it using a cholesterol-lowering drug called Ezetimibe.Marburg and Ebola hemorrhagic fevers are severe, systemic viral diseases affecting humans and non-human primates. They are characterized by multiple symptoms such as hemorrhages, fever, headache, muscle and abdominal pain, chills, sore throat, nausea, vomiting and diarrhea. Elevated liver-associated enzyme levels and coagulopathy are also associated with these diseases. Marburg and Ebola hemorrhagic fevers are caused by (Lake victoria) Marburg virus and different species of Ebola viruses, respectively.They are enveloped, single-stranded RNA viruses and belong to the family of filoviridae. Case fatality rates of filovirus disease outbreaks are among the highest reported for any human pathogen, ranging from 25 to 90% or more. But when Ezetimibe is given to patients with the Ebola virus, we see that the drug blocks the transmission of the virus to the body by delivering the virus to the immune system.Ezetimibe has a higher affinity for NPC1L1 receptor than cholesterol, and cholesterol has a higher affinity for NPC1L1 receptor than Ebola virus . In fact, if we want to show the percentage of desire for NPC1L1 receptor, it is as follows:
Ezetimibe> Cholesterol> Ebola virus
Keywords:Ebola-NPC1-Ezetimibe-NPC1L1-Cholesterol
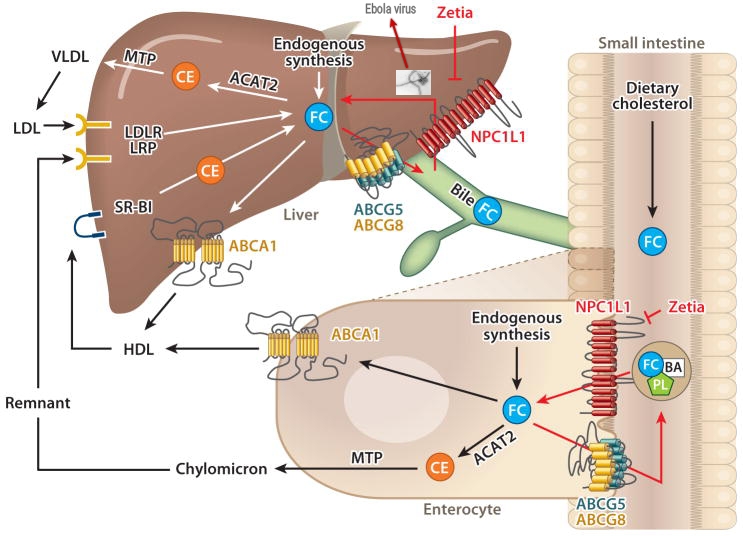
List of Abbreviations:EBOV: Ebola virus; MARV: Marburg virus; CM-C: Chylomicron cholesterol; GP: Glycoprotein; co-IP: Co-immunoprecipitation; Ctrl : Cell lysates lacking; NPC1: Niemann-Pick C1; NPC1L1: Niemann-Pick C1-Like 1; RAP: Receptor-associated protein; FC: Free cholesterol; BA: Bile acid; PL: Phospholipid; Ezetimibe: Zetia; CE: Cholesterol ester; ACAT2: Acyl-CoA:cholesterol acyltransferase 2; MTP: Microsomal triglyceride transfer protein; ABC: ATP-binding cassette; HDL : high-density lipoprotein; LDL: low-density lipoprotein; LDLR: LDL receptor; LRP: LDLR-related protein; VLDL: very low density lipoprotein
Introduction
Ebola virus (EBOV) and Marburg virus (MARV) are both members of the Filoviridae family of enveloped negative-strand RNA viruses and are the causative agents of a highly lethal disease for which no approved vaccines or treatments are currently available (Figure 1). Due to their virulence and biothreat potential, filoviruses are classified as category A pathogens. The ongoing EBOV epidemic in West Africa is the longest and most widespread filovirus outbreak on record.
When Ebola killed many people, people were found who survived Ebola. As more and more research was done on Ebola survivors, it led us to the hypothesis that Ebola survivors had hypercholesterolemia. It was here that a serious scientific attack was made against the treatment of Ebola using cholesterol.If we take a closer look at cholesterol transfer, we will find that liver cells, endothelium and macrophages are involved in cholesterol transfer. In fact, these cells are also target cells of the Ebola virus.Cholesterol is present in tissues and in plasma in the form of free or stored cholesterol, attached to long-chain fatty acids as cholesterol esters. In plasma, both forms are transported in lipoproteins. Cholesterol is an amphipathic lipid and an essential structural component of membranes that is important for maintaining their permeability and fluidity, and is the outer layer of plasma lipoproteins. It is made from acetyl coa in various tissues and is a precursor to all steroids, including corticosteroids, sex hormones, bile acids, and vitamin D. Cholesterol is found in animal foods such as egg yolks, meat, liver and brain because it is a metabolic product in animals. Plasma LDL is a means of supplying cholesterol and cholesterol esters to various tissues. Free cholesterol is transported by the HDL plasma through a process called reverse cholesterol transport from the tissues to the liver, where it is excreted either as free cholesterol or after it is converted to bile acids. Cholesterol is a major component of gallstones. Also, its main role in pathological processes is to act as a factor that causes atherosclerosis of vital arteries and, consequently, cerebrovascular, cardiac and peripheral vascular disease. Slightly more than half of the body’s cholesterol through biosynthesis and the rest through A normal diet is provided. The liver and intestines each make up about 10% of the total cholesterol synthesized in humans. All tissues with nucleated cells are able to synthesize cholesterol. Cholesterol is synthesized in the endoplasmic reticulum and cytosolic segments (Figure 2) [1-10].
Atherogenic potential of intestinally-derived lipoproteins. This schematic illustrates two mechanisms through which the entry of chylomicron cholesterol (CM-C) into the circulation can potentially play a role in atherosclerotic plaque formation. (1) The uptake of CM-C by the liver can lead to a shift in intrahepatic cholesterol metabolism that in turn causes either a downregulation of low-density lipoprotein receptor (LDL-R) activity, or/and an increase in hepatic very low-density lipoprotein-cholesterol (VLDL-C) secretion. Either of these events can lead to a rise in the steady-state plasma low density lipoprotein-cholesterol (LDL-C) concentration. (2) Upon entering the circulation, CM’s lose much of their triacylglycerol content, resulting in the formation of a much smaller, cholesterol rich remnant particle (CMr) that can permeate the vessel wall. Ordinarily, CMr particles are rapidly cleared from the circulation by the liver but in Type 2 diabetes and other disorders this clearance rate can be markedly delayed.
Ebola and Marburg filoviruses cause deadly outbreaks of haemorrhagic fever. Despite considerable efforts, no essential cellular receptors for filovirus entry have been identified.Ebola virus uses its glycoprotein (GP) to enter new host cells. During entry, GP must be cleaved by human enzymes in order for receptor binding to occur.Niemann-Pick C1 (NPC1), a lysosomal cholesterol transporter, is required for filovirus entry. NPC1 is a critical filovirus receptor. Human NPC1 fulfills a cardinal property of viral receptors. This receptor on hepatocytes and macrophages are actually located. This receptor as well entry cholesterol in these cells [11-14].
For example, a study conducted to treat Ebola with NPC1 receptor blockade was quite successful in mice but failed in humans (Figure 3).
NPC1 binds specifically and directly to a cleaved form of the Ebola virus glycoprotein. (A) Co-immunoprecipitation (co-IP) of NPC1 by EBOV GP. Magnetic beads coated with GP-specific monoclonal antibody KZ52 were incubated with detergent extracts containing no virus (None), uncleaved rVSV-GP, or cleaved rVSV-GPCL. The resulting control or glycoprotein-decorated beads were mixed with cell lysates containing human NPC1–Flag at pH 7.5 or 5.1 and 4°C. Beads were then retrieved and NPC1–Flag in the immune pellets and supernatants was detected by IB with an anti-Flag antibody. Pellets and supernatants were resolved on separate gels but exposed simultaneously to the same piece of film. (B) Reciprocal co-IP of GP by NPC1. Cell lysates lacking (Ctrl) or containing NPC1–Flag were incubated with anti-Flag antibody-coated magnetic beads. The resulting control or NPC1-decorated beads were mixed with detergent extracts of rVSV-GP or rVSV-GPCL at pH 7.5 and 4°C. Beads were then retrieved and GP or GPCL in the immune pellets and supernatants was detected by IB with an anti-GP antiserum. Pellets and supernatants were resolved on separate gels but exposed simultaneously to the same piece of film. Asterisks indicate bands detected non-specifically by the antiserum. (C) GPCL captures NPC1 but not NPC1-like1 (NPC1L1) in an ELISA. Plates coated with rVSV-GP or rVSV-GPCL were incubated with cell extracts containing NPC1–Flag or NPC1L1–Flag, and bound Flag-tagged proteins were detected with an anti-Flag antibody. Results (n=3) are representative of at least four independent experiments. (D) Cell extracts used in (C) were incubated with plates coated with an anti-Flag antibody or an isotype-matched control, and captured proteins were eluted and detected by IB with the anti-Flag antibody. Samples were resolved on the same gel. (E, F) NPC1L1 cannot support filovirus entry and infection. CT43 cells expressing NPC1L1–Flag were exposed to wild-type EBOV or MARV (E) or to recombinant VSVs (F), and infected cells were visualized and enumerated by fluorescence microscopy. Asterisks in (E) indicate values below the limit of detection. Scale bar, 20 μm. (G, H) GPCL but not GP captures affinity-purified NPC1–Flag in an ELISA. (G) NPC1–Flag was purified from CT43 CHO cell lysates by Flag affinity chromatography and visualized by SDS–PAGE and staining with Krypton infrared protein stain. Samples were resolved on the same gel. (H) ELISA plates coated with rVSV-GP or rVSV-GPCL were incubated with NPC1–Flag purified in (G), and bound Flag-tagged proteins were detected with an anti-Flag antibody. Results (n=3) are representative of at least four independent experiments. Error bars indicate s.d. Figure source data can be found in Supplementary data [15-17].
It was here that the hypothesis came to mind that we should look for a receptor other than NPC1 but related to cholesterol transfer. This is where the NPC1L1 receptor came into play ( Fig4 ). Different functions have been attributed to the NPC1L1 receiver. One function suggests that NPC1L1 is located not in the plasma membrane but intracellularly where it is thought to be involved in the cytosolic trafficking of cholesterol.In another report, a protein other than NPC1L1 is responsible for high cholesterol binding to the gut. But most agree that the NPC1L1 receptor acts as an LDL receptor. NPC1L1 is essential for intestinal cholesterol absorption, and is the target of ezetimibe, a cholesterol absorption inhibitor. NPC1L1 has been identified and characterized as an essential protein in the intestinal cholesterol absorption process. NPC1L1 localizes to the brush border membrane of absorptive enterocytes in the small intestine. Intestinal expression of NPC1L1 is down regulated by diets containing high levels of cholesterol.
Methods
When people with hypercholesterolemia are exposed to the Ebola virus, the virus blocks the cholesterol transport pathway, and as the sources of cholesterol become blocked, the liver begins to synthesize cholesterol, which is done by releasing stored cholesterol. These stored sources of cholesterol can be the gallbladder and liver, as well as tissues and even blood vessels. In fact, by binding to NPC1L1, the virus inhibits the transmission of cholesterol, and as a result, the liver needs cholesterol to survive itself and other organs, which it does by invoking cholesterol from these sources. This is where LDL plays by connecting to the NPC1L1 receiver.NPC1L1 may have evolved at two sites (apical membrane of enterocytes and canalicular membrane of hepatocytes) to mediate cholesterol uptake through a clathrin-mediated endocytic process, protecting the body against fecal and biliary loss of cholesterol.In fact, if a person with hypercholesterolemia becomes infected with the Ebola virus, stored cholesterol flows and prevents the virus from entering the target cell because cholesterol has a higher affinity for NPC1L1 than the virus. The result is that the virus is released into the immune system and antibodies are formed against the virus.In people with low cholesterol, it is the virus that binds to the NPC1L1 receptor and binds to the target cell, killing the cell. Ezetimibe (Zetia) is a selective cholesterol absorption inhibitor, which potently inhibits the uptake and absorption of biliary and dietary cholesterol from the small intestine without affecting the absorption of fat-soluble vitamins, triglycerides or bile acids (Figure 5).
The role of Niemann-Pick C1-Like 1 (NPC1L1) in cholesterol transport in the small intestine and liver. In the lumen of the small intestine, unesterified free cholesterol (FC) from dietary intake and biliary secretion is solubilized in mixed micelles containing bile acids (BA) and phospholipids (PL). This solubilization is critical for the diffusion of FC across the unstirred water layer to reach intestinal brush border membranes, where FC is taken up into enterocytes by the apically localized NPC1L1 protein. Ezetimibe (Zetia) can inhibit this NPC1L1-dependent cholesterol uptake. The majority of absorbed and endogenously synthesized cholesterol is transported to the endoplasmic reticulum, where it is converted to cholesterol ester (CE) by acyl-CoA:cholesterol acyltransferase 2 (ACAT2) and is then assembled into chylomicrons in a microsomal triglyceride transfer protein (MTP)-dependent manner for secretion into the circulation via the lymphatic system. Unesterified FC may be transported back to the intestinal lumen by the apically localized heterodimeric sterol transporter ABCG5/ABCG8 [ATP-binding cassette (ABC) transporters G5 and G8]. FC may also be transported into the circulation as a constituent of high-density lipoprotein (HDL) via ABCA1 located at the basolateral membrane of enterocytes. In the liver, cholesterol can be synthesized locally or taken up by hepatocytes from circulating lipoproteins such as low-density lipoprotein (LDL), HDL, and chylomicron remnants via LDL receptor (LDLR), HDL receptor scavenger receptor class B type I (SR-BI), and LDLR-related protein (LRP) localized at the basolateral membrane of hepatocytes. A large amount of FC is converted to bile acids for hepatobiliary secretion. A proportion of FC is esterified by ACAT2 and then packaged into nascent very low density lipoprotein (VLDL) particles in an MTP-dependent manner for secretion into the circulation as a constituent of VLDL. Unmetabolized FC can be transported to ABCA1 localized at the sinusoidal membrane of hepatocytes for the biogenesis of HDL or to ABCG5/ABCG8 localized at the canalicular membrane of hepatocytes for direct secretion into bile. In humans and nonhuman primates, NPC1L1 is also localized at the apical membrane of hepatocytes, where it may counterbalance the function of ABCG5/ABCG8 by transporting newly secreted biliary cholesterol back into hepatocytes, thereby preventing excessive loss of endogenous cholesterol.
However, Ezetimibe should be given to people with low cholesterol sources as well as people infected with the Ebola virus, as Ezetimibe is more affinity to NPC1L1 and does not allow the virus to bind to the NPC1L1 receptor, thus preventing the virus from entering the goal cell. In fact, it does what cholesterol does in people with hypercholesterolemia when they get the Ebola virus. In the pathology of the disease, two symptoms show the most: 1- destruction of macrophages 2- rupture of renal arteries.Regarding the destruction of macrophages, Filovirus infection requires fusion of the host cell and virus membranes, a process that is mediated by the envelope glycoprotein (GP), it is necessary to mention that in the transfer of oxidized LDL from tissues to vessels by macrophages, it transforms itself into a bubble. Because the virus enters the macrophage through the NPC1L1 receptor and transforms itself into a phagosome,After entering the phagosome of macrophages, the Ebola virus survived thereby destroying the macrophage.But in the case of ruptured arteries, we mentioned that the liver begins to synthesize cholesterol if its cholesterol sources are blocked, which is synthesized by releasing stored cholesterol sources. In people who have poor sources of cholesterol, by releasing stored cholesterol sources when it is not in the gallbladder, the liver and even the tissues and blood vessels, especially the renal arteries. This releasing of LDL from the arteries causes the arteries to become thinner, causing the arteries to rupture as blood passes through the arteries. Ultimately, this causes the body to rupture arteries to compensate for the lack of cholesterol [21].
Results
Based on the above, it can be concluded that Ezetimibe disrupts the transmission of Ebola virus in the body due to the high affinity of the NPC1L1 receptor. Thus, stored cholesterol goes to war with the Ebola virus, which has a higher affinity for the NPC1L1 receptor than the virus. In fact, the higher the stored cholesterol Resources, the more successful a person will be in fighting the Ebola virus, as it has been proven that people who survived Ebola virus had hypercholesterolemia.
Discussion
If Ebola patients receive Ezetimibe, the drug is delivered to the antibodies by blocking the NPC1L1 receptor for the Ebola virus. Of course, antibodies are the most effective defense against the Ebola virus. Ezetimibe is actually a supplier of antigen (Ebola virus) in the body. However, in a study of the genes of people who survived Ebola, this study showed that these people have hypercholesterolemia. We must note that by preventing the transfer of cholesterol, the liver begins to synthesize cholesterol, which is done through stored sources of this synthesis. Among the sources that are used are blood vessels that contain LDL levels, the use of these sources leads to thinning of blood vessels and ultimately leads to their rupture.
Conclusions
As described, it can be concluded that in patients with Ebola after receiving the drug Ezetimibe due to its high affinity for the NPC1L1 receptor, the virus prevents the virus from entering the goal cell and makes the virus visible to antibodies. It is also best taken with a reductase reducer to increase viral receptor blockade (NPC1L1).
Consent to publication
This manuscript is published with the aim that the Ebola virus is transmitted rapidly in the world and we are looking for a treatment for this disease.
Availability of data and materials
The comments made in this article are purely the opinion of the author and so far no experiments have been performed on either humans or animals.
Competing interests
The author declares no competing interests.
Acknowledgement
I thank Maedeh Khanifar for helping me in write this article.
- Role of Niemann-Pick c1 like1(NPC1L1) in Intestinal Sterol Absorption by Stephen D Turley.
- The target of ezetimibe is Niemann-Pick C1-Like1(NPC1L1), BY Margarita Garcia-Calvoa, JeanMarie Lisnock, Herbert G. Bull, Brian E. Hawes, Duane.
- Niemann-Pick C1-Like 1: A Key Player in Intestinal Cholesterol Absorption Haruaki Ninomiya Department of Biological Regulations, School of Health Science, Tottori University Faculty of Medicine, Yonago 683-8503.
- Ezetimibe Inhibits Hepatic Niemann-Pick C1-Like 1 to Facilitate Macrophage Reverse Cholesterol Transport in Mice Ping Xie, Lin Jia, Yinyan Ma, Juanjuan Ou, Hongming Miao, Nanping Wang, Feng Guo, Amirfarbod Yazdanyar, Xian-Cheng Jiang, Liqing Yu.
- Role of reverse cholesterol transport in animals and humans and relationship to atherosclerosis Daniel J. Rader1,2, Eric T. Alexander1,2, Ginny L. Weibel2, Jeffrey Billheimer1, George H. Rothblat2 1Institute for Translational Medicine and Therapeutics and Cardiovascular Institute, University of Pennsylvania School of Medicine, Philadelphia.2Children’s Hospital of Philadelphia.
- Host-Primed Ebola Virus GP Exposes a Hydrophobic NPC1 ReceptorBinding Pocket, Revealing a Target for Broadly Neutralizing Antibodies Zachary A. Bornholdt, Esther Ndungo, Marnie L. Fusco, Shridhar Bale, Andrew I. Flyak, James E. Crowe, Jr., Kartik Chandran, Erica Ollmann Saphire.
- Niemann-Pick C1 Like 1 (NPC1L1) Is the Intestinal Phytosterol and Cholesterol Transporter and a Key Modulator of Whole-body Cholesterol Homeostasis Harry R. Davis, Jr, Li-ji Zhu, Lizbeth M. Hoos, Glen Tetzloff, Maureen Maguire, Jianjun Liu, Xiaorui Yao, Sai Prasad N. Iyer, My-Hanh Lam, Erik G. Lund, Patricia A. Detmers, Michael P. Graziano, and Scott W. Altmann.
- Structure of human Niemann-Pick C1 protein by Xiaochun Li, Jiawei Wang, Elias Coutavas, Hang Shi, Qi Hao, and Günter Blobel.
- analogs with a reorganized azetidinone ring: Design, synthesis, and evaluation of cholesterol absorption inhibitions. Xianxiu Xu, Renzhong Fu, Jin Chen, Shengwu Chen and Xu Bai.
- Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, et al. (2012) Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 31: 1947-60.
- Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, et al. (2011) Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477: 340-3.
- Bornholdt ZA, Ndungo E, Fusco ML, Bale S, Flyak AI, et al. (2016) Host-Primed Ebola Virus GP Exposes a Hydrophobic NPC1 Receptor-Binding Pocket, Revealing a Target for Broadly Neutralizing Antibodies. mBio. 7: e02154-15.
- Hunt CL, Lennemann NJ, Maury W (2012) Filovirus entry: a novelty in the viral fusion world. Viruses 4: 258-75.
- Xie P, Zhu H, Jia L, Ma Y, Tang W, et al. (2014) Genetic demonstration of intestinal NPC1L1 as a major determinant of hepatic cholesterol and blood atherogenic lipoprotein levels. Atherosclerosis 237: 609-17.
- Davis HR, Altmann SW (2009) Niemann-Pick C1 Like 1 (NPC1L1) an intestinal sterol transporter. Biochim Biophys Acta 1791: 679-83.
- Jia L, Betters JL, Yu L (2011) Niemann-pick C1-like 1 (NPC1L1) protein in intestinal and hepatic cholesterol transport. Annu Rev Physiol 73: 239-59.
- Betters JL, Yu L (2010) NPC1L1 and cholesterol transport. FEBS Lett 584: 2740-7.
- Yu L (2008) The structure and function of Niemann-Pick C1-like 1 protein. Curr Opin Lipidol 19: 263-9.
- Ge L, Wang J, Qi W, Miao HH, Cao J, et al. (2008) The cholesterol absorption inhibitor ezetimibe acts by blocking the sterol-induced internalization of NPC1L1. Cell Metab 7: 508-19.
- Hofmann-Winkler H, Kaup F, Pöhlmann S (2012) Host cell factors in filovirus entry: novel players, new insights. Viruses 4: 3336-62.
- Stock I (2014) Marburg- und Ebola-Fieber. Erreger, Epidemiologie und Therapie [Marburg and Ebola hemorrhagic fevers--pathogens, epidemiology and therapy]. Med Monatsschr Pharm 37: 324-30.

Figures at a glance