Changing Trends of Surgical Approach of Primary Hyperparathyroidism in The Last Twenty-Years: From Bilateral Neck Exploration to Mini-Invasive Access
Received Date: June 10, 2021 Accepted Date: July 10, 2021 Published Date: July 12, 2021
doi: 10.17303/jspcr.2021.3.202
Citation:Enrico Battistella (2021) Changing Trends of Surgical Approach of Primary Hyperparathyroidism in The Last Twenty-Years: From Bilateral Neck Exploration to Mini-Invasive Access. J Surg Proce Case Rep 3:1-8.
Abstract
Purpose:Primary hyperparathyroidism (PHPT) represents the third endocrinopathy with an incidence about 25/100000 people. PHPT determines hypercalcemia that could be asymptomatic or symptomatic with various manifestations. The aim of this study is to explain our point of view based on our long experience in diagnostic procedure and surgical intervention.
Materials and Methods:This retrospective, single-center study included 301 patients with PHPT treated from January 1997 to December 2020. In all cases, measurement of intra-operative PTH was performed. Pre-operative diagnostic procedure performed included neck ultrasonography and technetium 99-m sestamibi imaging, in doubtful cases fine needle aspiration biopsy and 18F-Flurocholine (FCH) positron emission tomography (PET) were performed.
Results:Of the 301 patients included, 223 were women (75%) and 78 men (25%), with a mean age of 51.8 years. After 2009, a total of 219 surgical procedures were performed as minimal invasive parathyroidectomy and only in 9 cases bilateral neck exploration was done. Before 2009, we use only open approach (73 patients). Io-PTH assay showed a reduction in 262 cases (87%) but operative success was achieved in 283 cases (94,1%) thanks to the surgeon experience. A five-years follow-up was performed and patients with successful surgery did not show any signs or symptoms of PHPT.
Conclusion:The development of diagnostic tools that localize with high precision abnormal parathyroid gland combined to ioPTH enables the surgical treatment of patients with PHPT with focused approaches and excellent results that are stackable of bilateral neck exploration. When this methods fails, only experienced surgeon could solve this situation.
Keywords:Primary hyperparathyroidism; intra-operative PTH-assay; mini-invasive parathyroidectomy; bilateral neck exploration; endocrine surgery
Introduction
Primary hyperparathyroidism (PHPT) is a disease of the parathyroid gland (PG) and it represents the third endocrinopathy after diabetes mellitus and thyroid disease. The incidence is about 25/100000 people and as other endocrine disease, it is more frequent in females than males with a ratio 1/3, with a peak of incidence in the early post-menopausal [1,2].
PHPT causes an excessive production of parathormone (PTH) that determined hypercalcemia due to the stimulation to a higher bone reabsorption and an increased calcium reabsorption by renal tubule and by gut.
It is diagnosed through biochemical screening and appear an asymptomatic disordered related to hypercalcemia characterized by a histological pattern that included parathyroid adenomas (in >80% of cases), multiple adenomas and parathyroid hyperplasia (about 15%), finally parathyroid carcinoma (<1%) [3].
There are two types of PHPT: sporadic form (with no familiar history) and hereditary form with an incidence of no more than 10% in the PHPT population (MEN I, MEN IIa, MEN IV, familial hypocalciuric hypercalcemia, neonatal severe PHPT). Possible causes of primitive hyperparathyroidism are exposition to radiation in the neck area, treatment with lithium, and hereditary pattern [4,5].
Parathyroidectomy, the only curative treatment for PHPT, is recommended for patients with symptoms and for those with asymptomatic disease who are at risk of progression or have subclinical evidence of end-organ effects [6]. It is important to have a pre-operative imaging to keep the correct localization of the parathyroid gland because it permitted a mini-invasive approach.
In this case series, we explain our approach to the disease from diagnosis to surgical treatment, including intra-operative procedure performed, in over twenty-years’ experience.
Material and results
Demographic and clinical data were retrospectively entered in a computerized endocrine surgery registry for all patients who underwent surgery for PHPT at our institution. Our study included 301 patients with diagnosis of PHPT (78 males, 223 females, M: F=1:3), operated since 1997. We did not include patients affected by secondary and tertiary hyperparathyroidism. The average age at the time of the surgery was 51.8 (range 11-84 years).
Patients considered suitable for surgery and included in our study were symptomatic PHPT and, asymptomatic PHPT with age <50 years, persisted elevated serum calcium, vertebral fracture, nephrolithiasis or nephrocalcinosis, creatinine clearance of <60 ml/min, according to the American Association of Endocrine Surgeon Guidelines [6].
One or more imaging investigations were done before the hospitalization: neck ultrasonography (US) was performed in all patients while scintigraphy in 283 patients (94%). PTH-assay in fine needle aspiration biopsy (FNAB) during US was performed in 30 patients. In the last 3 years, we performed in 24 patients 18F-Flurocholine (FCH) positron emission tomography (PET) for doubtful position.
340 parathyroid glands were removed, 226 on the right (66,5%), 79 on the left (23,2%), and 35 ectopic (10,2%). The histological reports showed 221 single adenomas (65%), 71 multiple adenomas (21%), 41 hyperplasia (12%), 7 parathyroid carcinomas (2%). Parathyroidectomy, homolateral thyroid lobectomy and lymph node dissection was performed in patients with parathyroid carcinoma.
The surgical approach was chosen between bilateral neck exploration (BE) and mini-invasive parathyroidectomy (MIP) considering the results of the pre-operatory investigations. It should be mention that we started to perform MIP since 2009, so we have a first group that included patients from 1997 to 2009 that underwent to BE in any case (GROUP A=73 patients), and a second group that included patients from 2009 to 2020 that were approached with MIP or BE (GROUP B=228 patients).
In GROUP A, BE was considered the gold standard surgical approach and for this, it was performed in all cases (73 pts=100%). In GROUP B, mini-invasive approach was the common surgical technique, and it was performed in 219 cases (96%) and only in 9 cases (4%) BE was chosen from the beginning for indeterminate localization in 3 cases and for concomitant thyroid carcinoma in 6 cases. Conversion to bilateral exploration was due to impossibility to recognize the abnormal parathyroid gland in 11 patients despite the pre-operatory imaging (5%).
Surgical failure (defined as the persistence of hypercalcaemia and hyperparathyroidism) happened in 7 cases (9,6%) in GROUP A, while in 11 cases (4,7%) in GROUP B. In GROUP B all the failed procedure appeared when doubtful pre-operative localization was present and BE or conversion to BE was necessary.
In GROUP A, complications reported were a transient state of hypocalcaemia in 6 cases (8%), neck haematoma in 3 cases (4%), and recurrent laryngeal nerve injury in 3 cases (2,7%).
In GROUP B, hypocalcaemia was not evidence in the first post-operatory, neck haematoma and recurrent laryngeal nerve injury was complained in 2 cases (0,9%).
In all patients, we performed PTH assay the day of hospitalization and 10 minutes after abnormal PG removal.
The io-PTH assay showed a reduction in 262 cases (87%): more precisely there is a decline higher the 70% in 247 cases (82%), a decline of 40-70% in 45 cases (15%) and a decline of 20-40% in 9 cases (3%). In 39 cases there was an insignificant reduction of PTH in the blood test (13%).
In all the patients with a reduction of PTH value higher than 40% (169 patients, 84%), we noticed that calcium level was normalized in first post-operative day and they showed a normal PTH level and a normal range of calcium serum.
The average length of staying (LOS) of GROUP A was 3 days (3-5 days), while average LOS of GROUP B was 2 days (1-3 days).
During a five-year follow-up consisting in an endocrinological visit with biochemical evaluation (serum calcium level and PTH-assay) every six months for the first year and once for the following 4 years, the patients that underwent to a successful parathyroidectomy did not presented any type of recurrence of PHPT. In the group of patients with surgical failure (18 cases), three patients underwent to a new surgical approach after localization study with 18F FCH-PET and clinical success was obtained. A non-surgical management was used for the others 15 patients using Cinacalcet or Raloxifene depending on endocrinological indications.
Discussion
PHPT consisted in an inappropriate excessive production of PTH resulting in hypercalcemia. In the moment of the diagnosis, 85% of patients are completely asymptomatic or lightly symptomatic, so called biochemical hyperparathyroidism [7,8]. The presence of symptoms is related to the level of calcium concentration and the increased level of PTH due to the loss of regulating function of parathyroid cells. When hypercalcemia is high enough, generally other 12 mg/dL (range 8,5- 10,5 mg/dL), or if is increased rapidly in few days, symptoms are various and included clinical manifestation (polyuria, polydipsia), neurological manifestations (depression, psychosis, confusion, delirium, stupor, lethargy), kidney involvement (renal calcolosis, nephrocalcinosis, kidney failure), gastro-intestinal manifestations (dyspepsia, nausea, pancreatitis, stypsis), asthenia [9].
The recommended evaluation of a patient with suspected PHPT included serum PTH, calcium, phosphate, alkaline phosphatase activity, renal function tests, 25- hydroxyvitamin D. Another test that should be included is 24-hour urine for calcium and creatinine [5,10].
The diagnostic imaging that should be done is focalized to find the correct localization of pathological parathyroid.
The most common localization study is neck ultrasound (US). Normal parathyroid glands usually are not recognizable while thanks to the improvement of technology hyperplasic parathyroid gland are viewable since 5 mm diameter. The position and the number of parathyroid glands is variable, and it is important to consider all the possibility. Adenomatous parathyroid glands appear as nodular lesions especially hypoechoic. They can be also with liquid area inside (4%) or with calcification (2%), or with cystic aspect. Parathyroid glands usually present mark shape or thin “like a cigar” with well-defined boundaries due to the hyperechoic capsule that permits to distinguish from the thyroid tissue. The sensibility of US reported in literature arrived to the 85%, range 60%-95% depending on the dimension of the gland and the radiologist experience [4,11].
Another important diagnostic tool to localize parathyroid gland is technetium 99-m sestamibi imaging (SPET). This is the first radiopharmaceutical used to the localization of the parathyroid glands. This modality achieves sensibility for finding abnormal parathyroid glands of 69-91% but it can visualize only pathological PG because the normal one is too small to be viewable [11,12]. In our practice, we performed this two diagnostical approach because they guarantee in combination a high sensibility of the correct positioning of abnormal PG. PTH quantitation in FNAB was performed in 30 cases and in 95% of cases was a positive predictive value.
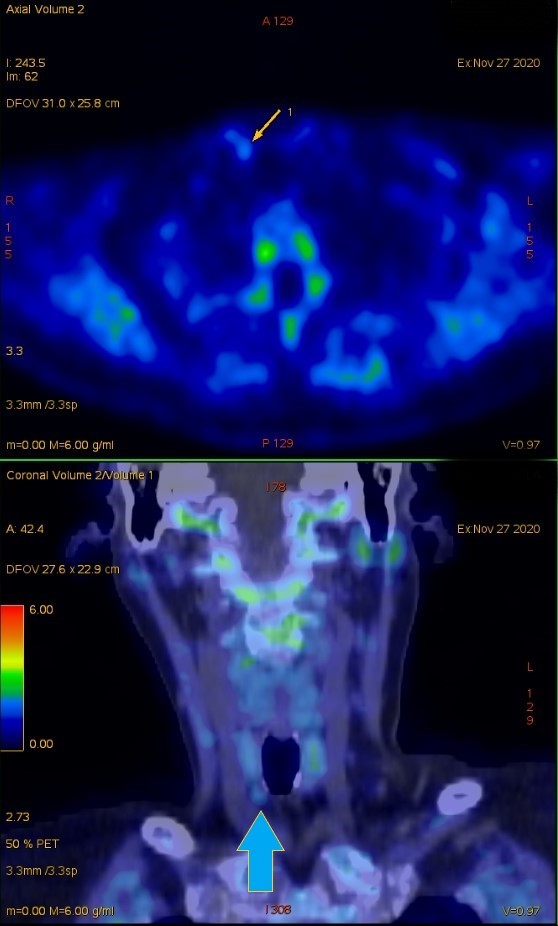
Recently, in Literature, it has been reported that 18F FCH-PET with computed tomography (CT) is more accurate than conventional morphological and functional imaging modalities for the detection of parathyroid glands. In our analyses, considering the cost effectiveness, 18F FCH-PET should be considered in case of doubtful localization of abnormal PG to permit a mini-invasive surgery [13]. Since the 2017, we performed 18F FCH-PET in 24 cases with a correct localization in 23 (95.8%) (Figure 1).
Another diagnostic instrument is 4D-CT that is a new modality of parathyroid imaging and it is based on the features of perfusion of parathyroid adenomas. The fast wash-in and wash-out of adenomas can be analyse with a rapid sequence of images with the result of multiplanar image highly detailed that can reveal abnormal parathyroid distinguishing from thyroid tissue and lymph-nodes. In literature, studies support the utility of this method in case of the reoperation of the neck. 4D-CT has an 86% of right primary positioning of abnormal parathyroid gland and gives the possibility to discover multiglandular disease or ectopic parathyroid gland. The disadvantage is the exposition to a high volume of radiation and that is why the indication to use it should be given only in difficult case [7,10,14].
To complete the evaluation of the disease, it is important to include abdominal imaging (abdominal x-ray or ultrasound) and vertebral imaging. Indeed, many studies show that patients with asymptomatic PHPT have vertebral involvement and renal stones or nephrocalcinosis [15,16].
The parathyroidectomy represents the definitive treatment for PHPT, but this procedure requires an expert surgeon due to the small dimension of PG and the variability of localization of PG [17,18]. The percentage of success in patients affected by parathyroid adenomas reaches the 95% of cases [11,18]. The rate of persistence of disease (hypercalcemia within 6 months from the surgery) or recurrence of disease (hypercalcemia after 6 months of surgery) is about 10-20% [11].
For the surgeon, pre-operatory imaging is very important to decide the best operative strategy. The chosen of the surgical approach (open surgery or mini-invasive surgery) depends on adenoma sizes, the localization, the presence of pathological thyroid, the presence of previous cervicotomy and the experience of the equipe.
The ectopic parathyroid localization is the 10-20 % of all parathyroid gland and they can be retroesophageal, between trachea and oesophagus, behind the farinx, and inside the thyroid gland, the thymus, and the mediastinum tissue [19].
Thanks to the short half-life of the molecule, the variation of PTH value can be considered significative in few minutes after parathyroidectomy and can reduced substantially times of classical exploration of the neck region. Some authors showed that the PTH value decrease only after five minutes from removal of parathyroid gland. The surgery became faster, safer, and less expensive than before [20.21].
Traditionally the approach to the parathyroid surgery includes bilateral exploration of thyroid lodge and the superior mediastinum, starting from the normal positions of the four parathyroid glands following the migration lines of the third and fourth pouches, including the intra-thyroidal site. This is important to avoid the missed finding of a second adenomas, in a normal or ectopic side, a supernumerary gland and to treat adequately a pluriglandular hyperplasia with a cure rate of the 90-95% in experienced hands. The traditional bilateral neck exploration resulted useless in the 80% of cases with a complication rate of 1-3 % [22,23].
We performed mini-invasive approach, as described by Miccoli et al., in 219 patients (72%) since 2009 with a clinical success in 208 (95%). We use systemically this method to approach PHPT surgery, the principal indication for being eligible for a focused approach is a successful pre-operative localization because abnormal parathyroid gland is approached with a focused mini-incision [24,25].
The main advantage of intra-operative PTH assay (io-PTH assay) resulted in the exploration of only one side of the neck thanks to the possibility of predicting an accurate surgical removal, excluding the presence of pathological parathyroid tissue. The kinetics of elimination of PTH has a biphasic trend: in the first 2-3 minutes there is a rapid decrease of PTH concentration in blood sampling, after it is possible to assist to a following phase of decrease slower than the first one. This happens because PTH is composed by more unites. Especially, the N-terminal portion that is biologically active part has a half-life very short. Thanks to this sub-unit, io-PTH assay is commonly used in intra-operative identification [25].
In Literature is reported that there is a clinical sensibility of the 85% in io-PTH assay when a reduction higher than 50 % of the starting value of PTH after five minutes of the surgical excision is marked in a blood sampling while after 10 minutes the sensibility reaches the 97%, we prefer for this reason the assay after 10 minutes [26]. In some studies, the value of PTH was related to the histology of the lesions: the PTH assay was higher in parathyroid carcinoma than in other abnormal parathyroid tissue.
The surgical approach must be traditionally open in this situation: absent pre-operatory localization, suspected pluri-gland interesting, suspected parathyroid carcinoma, PHPT Men-related, PTPH related with goitre or thyroid cancer [4].
The impossibility to localize with pre-operatory imaging the PG involves the necessity to explore all the PG including an area extending from the carotid bifurcation to the mediastinum. The technique of exploration includes the section of upper thyroid peduncles, the medialization of thyroid lobes, the section of medium thyroid vein. In addition, a trained eye is necessary to recognized normal PG that appears tan in colour with a diameter of 4-6 mm surrounded with an adipose capsule.
We have founded that in all patients with io-PTH assay showed a decline higher than 40% of the starting value, calcium serum levels were normalized. A decline smaller than 40% or no decline have to be considered a surgical failure. When the result is doubtful, it is important to include the possibility of an error of the blood sampling. Some studies showed a slow decrease of PTH value due to the manipulation during the surgical act.
Conclusion
Parathyroidectomy is the unique possibility to solve PHPT and to avoid fatal complications, as we previous described [26]. Mini-invasive approach is the technique of choice when localization is well-defined thanks to the use of ioPTH-assay and the improvement of diagnostic tools. When the pre-operatory imaging is doubtful for localization of abnormal PG or PHPT is related to thyroid disease or genetic form, the gold standard technique remains bilateral neck exploration. In most of the case, io-PTH assay could confirm the correct surgical approach and it can be essential in cases of multiple adenomas. The limit is still the impossibility to suggest what to do when no variations of PTH value is registered and, in this situation, only the experience of the surgeon can solve this question.
Funding sources
This research did not receive any specific grant from funding agencies in the public. Commercial or not-for-profit sectors.
Declaration of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals.
Informed consent
For this type of study, formal consent is not required.
- YEH, Michael W (2013) Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. The J Clin Endocrinol Metabol 3: 1122-9.
- SILVERBERG, Shonni J (1999) A 10-year prospective study of primary hyperparathyroidism with or without parathyroid surgery. New England J Med 17: 1249-55.
- DELELLIS Ronald A, MAZZAGLI Peter, MANGRAY Shamlal (2008) Primary hyperparathyroidism: a current perspective. Archives pathol lab med 8: 1251-62.
- FRASER Sheila (2017) Surgical management of parathyroid disease. Surgery (Oxford) 10: 582-8.
- WALKER Marcella D, SILVERBERG Shonni J (2018) Primary hyperparathyroidism. Nature Reviews Endocrinology 2: 115.
- WILHELM, Scott M (2016) The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA surgery 10: 959-68.
- CALLENDER Glenda G, UDELSMAN Robert (2014) Surgery for primary hyperparathyroidism. Cancer 23: 3602-16.
- BABWAH, Feaz, BUCH Harit N (2018) Normocalcaemic primary hyperparathyroidism: a pragmatic approach. J clin pathol 4: 291-7.
- BILEZIKIAN John P (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. The Journal of Clinical Endocrinology & Metabolism 10: 3561-9.
- KHAN AA (2017) Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporosis International 1: 1-19.
- EGAN Richard J, SCOTT-COOMBES David M (2018) The surgical management of sporadic primary hyperparathyroidism. Best Practice & Research Clinical Endocrinology & Metabolism 6: 847-59.
- NORTON Kathryn S (2002) The sestamibi scan as a preoperative screening tool. The American surgeon 9: 812.
- EVANGELISTA Laura (2020) 18 F-choline PET/CT and PET/MRI in primary and recurrent hyperparathyroidism: a systematic review of the literature. Annals of Nuclear Medicine 2020: 1-19.
- STARKER Lee F (2011) 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Annals of surgical oncology 6: 1723-8.
- REJNMARK Lars, VESTERGAARD Peter, MOSEKILDE Leif (2011) Nephrolithiasis and renal calcifications in primary hyperparathyroidism. The Journal of Clinical Endocrinology & Metabolism 8: 2377-85.
- MOSEKILDE Leif (2008) Primary hyperparathyroidism and the skeleton. Clinical endocrinology 1: 1-19.
- GIMM Oliver (2019) Training in endocrine surgery. Langenbeck’s archives of surgery 8: 929-44.
- BERGENFELZ Anders (2007) Scandinavian Quality Register for Thyroid and Parathyroid Surgery: audit of surgery for primary hyperparathyroidism. Langenbeck’s archives of surgery 4: 445-51.
- NOUSSIOS G, ANAGNOSTIS P, NATSIS K (2012) Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Experimental and clinical endocrinology & diabetes 10: 604-10.
- CHRISTOFORIDES Christos (2019) Surgical treatment in patients with single and multiple gland primary hyperparathyroidism with the use of intraoperative parathyroid hormone monitoring: extensive single-center experience. Hormones 3: 273-9.
- HELBROW J (2016) The use of intraoperative parathyroid hormone monitoring in minimally invasive parathyroid surgery. The Annals of The Royal College of Surgeons of England 7: 516-9.
- KIERNAN Colleen M (2019) Bilateral neck exploration for sporadic primary hyperparathyroidism: use patterns in 5,597 patients undergoing parathyroidectomy in the collaborative endocrine surgery quality improvement program. Journal of the American College of Surgeons 4: 652-9.
- RUSSELL CFJ, DOLAN SJ. LAIRD JD (2006) Randomized clinical trial comparing scan‐directed unilateral versus bilateral cervical exploration for primary hyperparathyroidism due to solitary adenoma. British J surg 4: 418-21.
- MICCOLI Paolo (2003) Minimally invasive video assisted parathyroidectomy (MIVAP). European Journal of Surgical Oncology (EJSO) 2: 188-90.
- UDELSMAN Robert (2014) The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. The J Clin Endocrinol Metabol 10: 3595-06.
- BARCZYNSKI Marcin (2007) Intraoperative parathyroid hormone assay improves outcomes of minimally invasive parathyroidectomy mainly in patients with a presumed solitary parathyroid adenoma and missing concordance of preoperative imaging. Clinical endocrinol 6: 878-85.
- BATTISTELLA Enrico, POMBA Luca, TONIATO Antonio (2020) Acute heart failure in parathyreotoxicosis. Endocrine 2020: 1-2.

Figures at a glance