Esthesioneuroblastoma
Received Date: January 26, 2022 Accepted Date: February 26, 2022 Published Date: February 28, 2022
doi: 10.17303/jocr.2022.3.102
Citation:Gharnati K (2021) Esthesioneuroblastoma. JJ Oncol Clin Res 3: 1-11
Abstract
Introduction:Esthesioneuroblastoma (ENB) is a rare malignant tumor developed at the expense ofthe neural-olfactory epithelium, and it is among the rarest cancer of nasal cavity. It is usually manifested by rhinological symptoms, the oculardamage may be inaugural or appears during the evolution of the secondary orbital damage. Computed tomography and magnetic resonance imaging allow a very precise general and loco-regional assessment. The diagnosis is anatomo -pathological.and treatment usually relies on surgery and radiotherapy
Materials and Methods:retrospective study of 12 cases within ENT department of the CHU HASSAN II of FEZ over a.period of 15 years
Results:The average age of our patients was 45 years without gender predominance. The average consultation period was 8months. Rhinosinus syndrome was the predominant clinical symptom, sometimes associated with ophthalmologic or neurological symptoms. All the patients benefited from a radiological assessment which allows to objetify the tumor as well as itslocoregional extensions. Four cases of intracranial expansion have been detected. Of the 12 cases, 10 patients received surgical treatment (either endonasal removal for six patients, combined way for three patients, or external way (paralateronasal type of Moure) forone patient) followed by complementary radiotherapy. Evolution has been satisfactory. In the remaining 2cases, treatment was only palliative (chemotherapy or radiotherapy) due to the extension of the tumor
Conclusion:Esthesioneuroblastoma (ENB) is a rare tumour, first described by Berger in 1924; it mainly affects men and usually occurs during the second and third decades. Clinicaly , it’s revealed most often by rhinological symptoms (uniform or bilateral nasal obstruction, epistaxis, anosmia). Neurological symptoms are common and ophthalmologic manifestations, such as exophthalmia, reflect tumor extension into the orbital. The diagnosis can only be made by anatomopathology. Treatment is based on surgical removal combined with radiochemotherapy.
Keywords:Esthesioney\uroblastoma; Nasal Obstruction; Epist axis; Surgery; Radiotherapy
Introduction
Esthesioneuroblastoma or olfactory neuroblastoma is a rare malignant tumor of the nasal cavities, developed at the expense of the olfactory epithelium [1,2]. Since its first description by Berger and Luc in 1924 as olfactory esthesioneuroepitheluim [3]. Limited series have been reported in the literature reflecting the difficulties of the diagnosis.
Through a retrospective study from January 2004 to December 2019, we will analyze a series of 12 patients with esthesioneuroblastoma who were collected at the ENT department of the CHU Hassan II of Fez.
The objective of our work is to study the different epidemiological, clinical and therapeutic parameters of this disease, and then we will use the literature as a foundation to make the point of the etiopathogenic hypotheses, the diagnostic means and the therapeutic modalities available to us for the management of these tumors.
Materials and Methods
This is a retrospective study spanning 15 years within the time frame of 2004 and 2019, involving 12 patients from the ENT department of the CHU Hassan II of Fez. Cases included in our study are men and women of different ages, who have been seen and treated for esthesioneuroblastoma at the ENT department of the CHU Hassan II of Fez.
Results
Between 2004 and 2019, we had the opportunity to treat 12 cases of esthesioneuroblastoma. There were 5 men and 7 women. The patient’s age ranged from 26 to 70 years with a mean of 48 years. The average consultation period was 8 months with extremes ranging from 2 months to 14 months. Almost all the patients showed symptoms of nasal obstruction and epistaxis followed by anosmia, face swelling and Rhinorhea in half of the cases. On the other hand, ophthalmologic signs were observed in three cases.
Clinical examination via the Endoscopy revealed the tumor and allowed us to do the biopsy which confirmed the diagnosis.
The radiological assessment (CT and/or MRI) revealed the tumor and its loco-regional extensions. Two cases of intracranial expansion have been identified.
An extension assessment has been realized for all our patients to establish a TNM classification: the majority of the cases had tumors classified between T2 and T3 (6 cases), 2 cases classified as T1 and 4 cases as T4. Cervical lymphadenopathy was found in 2 cases and distant metastases in only one case.
Of the 12 cases, 10 patients received curative treatment (first surgery followed by radiotherapy of 50-60Gy) using either the endonasal way for 6 patients, paralateronasal of Moure way for only onepatient or combined wayfor 3 patients. For the other 2 patients the lesion was invading adjacent structure, and they have benefited of palliative treatment: chemotherapy included cyclophosphamide (650 mg/m2) with vincristine (1. 5 mg/m2 with a maximum dose of 2 mg/m2).
The majority of patients have progressed well after five years of decline.
Discussion
Esthesioneuroblastoma is a rare tumor which represents 3% of all nasal tumors [2, 4]. In almost all published series, the authors report a small number of patients treated in the same institution, and the dispersion of these cases over time (often over a long period of time). It is a tumor that occurs at all ages with 2 frequency peaks, one between 11 and 20 years, the other between 50 and 60 years. It affects both sexes with a slight male predominance.
Histopathogenism of esthesioneuoblastomas is little known although Volrath and Altmannsberger may have induced neurofactory tumors using nitrosamines [6, 10]. The role of viruses, especially adenoviruses, is not clearly established in their carcinogenesis. However, on tumors developed spontaneously in cats, viral sequences have been found in the genome of tumor cells [10].
In a study analyzing the cytogenetic characterization of one case, numerous chromosomal aberrations were reported mainly involving chromosomes 2q, 5, 6q, 17, 19, 21q and 22, as well as Trisomy 8 [11]. Another study reported the presence of deletion of chromosomes 1p, 3p/q, 9p and 10p/q and amplifications of 17q, 17p13, 20p and 22q [12].
Ethesioneuroblastoma etiopathogenesis makes us discuss their membership in the PNET (Peripheral Neuro-Ectodermal Tumors) family to be discussed because of the frequency of T (11.22) translocation reported in Ewing's sarcoma [13].
The clinical manifestations of Ethesioneuroblastoma can't claim any sign of its own, especially since several symptoms can be associated, and often reflect an extensive intranasal process [10, 14, 15]. A well-conducted clinical examination of the ENT sphere is required to establish an early diagnosis.
Clinical Presentation
Clinical signs are dominated by either nasosinus symptoms or by objectifying the externalization of the lesional process beyond the nasosinus cavities. The fortuitous discovery on systematic histological analysis of a polypectomy is rare.Cervical lymphadenopathy is exceptional [4, 16, 17]
The symptoms are often late and especially not specific to a malignant process. Their banal nature and the high frequency of inflammatory or infectious pathologies of the nasosinus cavities explain that the diagnosis of these tumors is often suspected in the presence of fortuitously based on imagery [16,18]. Because of these non specific symptoms, certain characteristics must be taken into consideration: the one-sidedness, at least at the beginning, and the age of the manifestations that progressively lead to a worsening of the symptoms.
The esthesioneuroblastoma is characterized by high clinical variability and manifests itself in 3/4 of cases as ENT call signs [19, 20]. Eye signs are associated in 11% of cases [13, 19].
The CT/MRI pair allows the precise assessment of tumor extension. Indeed, MRI is crucial to clarify orbital and endocranial extension and also to differentiate between tumor mass and inflammatory retention. In advanced forms, the MRI aspect is a dumbell-shaped tissue process centred in the upper nasal cavity and extending into the intracranial [21,22].
Based on the extension, Kadish proposed (in 1976) a classification with three clinical stages [24]:
-Stage A: Tumor limited to the nasal cavity.
-Stage B: Tumour limited to the nasal cavity and sinuses.
-Stage C: Tumour extended beyond the nasal cavities and sinuses.
This classification was modified by Morita in 1993 [25] More recently Dulguerov [26] proposed a more accurate classification based on the TNM classification and using CT and MRI:
• T1: Tumor involving the nasal cavity and/or paranasal sinuses (excluding sphenoid), sparing the most superior ethmoidal cells.
• T2: Tumor involving the nasal cavity and/or paranasal sinuses (including the sphenoid), with/without extension to or erosion of cribiform.
• T3: Tumor extending into orbit or protruding into anterior cranial fossa, with/without dural invasion.
• T4: Tumor involving the brain.
Pathology
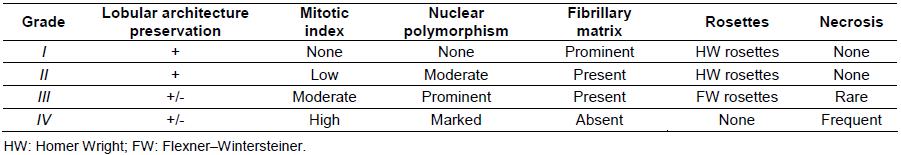
The histopathological aspect of esthesioneuroblastoma may be confusing with some small cell naso-sinusal tumors, especially in less differentiated forms. Immunohistochemistry is therefore a great help. In differentiated forms, the histological study shows lobules separated by conjunctivo-vascular partitions. Small to medium tumor cells have most often a roundnucleated nucleus and a clearly visible chromatin. The cytoplasm, which is not very abundant or moderately abundant, is poorly limited. Mitotic activity is highly variable [24, 27, 28]. Less frequently, the tumor is poorly differentiated, made up of diffuse layers of lymphocytoid cells, the tumor stroma is not very abondant and contains a prominent capillary network. The existence of a fibrillar fund -cytoplasmic, Flexner rosettes or Homer pseudorosettes -Wright (HW) is very revealing [29]. Hyams described a 4-grade histopathological classification system that relies primarily on the level of cell differentiation, the presence of neuronal stroma, the number of mitosis and the degree of necrosis (Table I [30]).
Treatment
Due to the rarity of esthesioneuroblastomas, the main source of assistance in making therapeutic decisions is the analysis of the results obtained by the authors who published their cases [30, 31, 32].
There is no standardized management of these tumors. The difficulty in establishing a better therapeutic strategy relies mainly in the small number of patients treated in the same institution, and in the dispersion of these cases over time (often over a long period of more than 20 years), which leads to a heterogeneous results [32,33].
Traditional treatment strategies are based on surgery or radiation therapy as single or combined modalities. More recently, chemotherapy has been introduced into the therapeutic arsenal of these tumours. Although there is a favourable consensus on the need for surgery, there is no agreement on the most appropriate surgical technique or on the use of complementary therapeutic methods [33, 34].
There is no standard surgical approach, however, there are two objectives: On the one hand, the possibility of controlling the entire anatomical limits of the tumor and the screened blade; On the other hand, carrying out a truly carcinological removal in monobloc, avoiding if possible Tumor fragmentation or excision by fragmentation [30]. There are basically three approaches: craniofacial, transfacial, and currently endonasal surgery is increasingly being used mainly in Kadish stages A and B [35]. The first surgical pathway is either transfacial performing a paralatero-nasal rhinotomy (for Kadish stages A and B), or by the upper subfrontal way if the base of the skull is reached [35, 36].
In the case of an orbital extension, attitudes are extremely nuanced, but most surgical teams are currently conservative towards the eyeball; due to the lack of significant differences in survival or recurrence rates when exempted. Esthesioneuroblastoma has a high local failure rate. As a result, most institutions have adopted surgical resection followed by postoperative radiation therapy as a standard treatment approach [35].
Postoperative radiation therapy has been shown to improve local disease control. However, for early-stage disease (Kadish A) with negative resection margins, the role of postoperative radiation is still questionable and surgery alone may be sufficient [37, 38]. The dose of radiation therapy used usually ranges from 55 to 65 Gy [39]. Due to the complexity of the anatomy and the location and proximity of various critical structures, there was always a concern about potential complications of adjuvant radiation; However, with the advancement of radiation technologies, compliant techniques such as Intensity Modulated Radiation (IMRT) and Proton Beam Therapy have shown better results in improving local control and minimizing toxicity and complications of nearby critical structures. [13,40]
The philosophy of treatment chemotherapy patients with esthesioneuroblastoma is based on the premise that these tumors share some histological features with other chemosensitive neural crest tumors (for example neuroblastomas, high-grade neuroendocrine carcinomas and PNETs) [41]. This theory has been proven by a variety of published retrospective analyses [42,43]. While another study has suggested that perioperative chemotherapy may be harmful [44].
The most commonly used schemes Cyclophosphamide (650 mg/m2) with vincristine (1. 5 mg/m2 with a maximum dose of 2 mg/m2) every 3 weeks for a total of 6 cycles [35].
Despite treatment, esthesioneuroblastoma remains a malignant tumor with a fazzy prognosis, since the overall survival at 5 years is of the order of 50%, and local or locoregional recurrences are very common [35].
Factors that affect the prognosis include:
➢ Local extension assessed according to the Kadish classification
➢ The histopathological grade of Hyams[30].
➢ Age: the prognosis would be better in a young person after adjustment on the stage. General condition and weight loss at diagnosis would rather be related to treatment tolerance and the risk of complications [45].
➢ Presence of cervical lymphadenopathy when the desease is discovered :
- A meta-analysis carried out in 2008 found that the disease control was 29% in patients with lymph node invasion, compared with 64% in the opposite case [10].
- Survival at 5 years is 0% if lymphadenopathies are present, compared to 65% if not [13].
➢ The presence of distant metastases: indicates a very disappointing prognosis [13, 35].
➢Diffuse marking at the PS 100and a low proliferation index to Ki 67: correlated with a better prognosis [35]
Conclusion
Esthesioneuroblastoma is a rare malignant tumor of the olfactory placode with an unknown etiology. It is characterized by clinical polymorphism, and a banality of symptoms that cause patients to reach advanced stages with significant locoregional invasion. Imaging (CTM and/or MRI) often makes it possible to evoke the diagnosis. It is an essential contribution to the evaluation of the pre-therapeutic, the determination of surgical tactics, and serves as a reference for assessing therapeutic response.
The precise diagnosis can only be made by anatomopathology. The treatment is not yet codified, but the radio surgical association seems to give the best chance of survival. Chemotherapy is reserved for advanced stages of the disease, inoperable tumours and incurable recurrences. Despite treatment, esthesioneuroblastoma remains a malignant tumour with a fuzzy prognosis, as the overall survival at 5 years is around 50%, and local or locoregional recurrences are very common.
- Taneja AK, Reis F, Queiroz LS, Araújo Zanardi V (2009) Esthesioneuroblastoma Arq Neuropsiquiatr 67: 704-6.
- Martel J, Darrouzet V, Duclos JY, Bebear JP , Stoll D (2000) Olfactory esthesioneuromas. Rev Laryngol Otol Rhinol 121: 227-36.
- Berger L, Luc R (1924) L’esthesioneuroblastome olfactifBull Ass Fran Cancer 13: 410-21.
- Zrara I, Al Bouzidi A, Rimani M, Azendour B, Labraimi A, Ben Omar S (1998) Olfactory esthesioneuromas (esthesioneuroblastomas) apropos of two clinical cases Médecine du Maghreb n ° 70.
- Takayuki Nakagawa (2017) Endoscopic endonasal management of esthesioneuroblastoma: A retrospective multicenter study ANL-2286.
- Gaye PM, Mesbah L, Kanouni L, Benjaafar N, El Gueddari BK (2010) Esthésioneuroblastome olfactif : expérience de l’institut d’oncologie de Rabat et revue de la littérature. J Afr Cancer 2: 36-40.
- Lapierre A, Selmaji I, Samlali H, Brahmi T, Yossi S (2016) Esthesioneuroblastoma: retrospective study and review of the literature.EMC CANRAD-3430.
- Chahed H, Kedous S, Zainine R, Daouadi A, Mediouni A, et al. (2014) Esthesioneuroblastoma: diagnostic dilemma and therapeutic challenges. J Tun orl: 3.
- Kermani W, Bouattay R, Zaghouani H, Belakhder M,Ben Ali M,et al. (2014) Olfactory esthesioneuroblastoma: about 7 cases. J. Tun orl: 31.
- Capelle L, Krawitz H (2008) Esthesioneuroblastoma: A case report of diffuse subdural recurrence and review of recently published studies Journal of Medical Imaging and Radiation Oncology 52: 85–90.
- Holland H, Koschny R, Krupp W, Meixensberger J, Bauer M, et al. (2007) Comprehensive cytogenetic characterization of an esthesioneuroblastoma. Cancer Genet Cytogenet 173: 89–96.
- Bockmühl U, You X, Pacyna-Gengelbach M, Arps H, Draf W, Petersen I (2004) CGH pattern of esthesioneuroblastoma and their metastases. Brain Pathol 14: 158–63.
- Ahmed S (2018) Abdelmeguid Olfactory Neuroblastoma. Current Oncology Reports (2018) 20: 7
- Haroussou JL, Mechinaud, Rialland X, Milpied N, Nomballais F (1988) Place de la chimiothérapie dans le traitement de l’esthésioneuroblastome de l’enfant à propos de 3 observations Ann Pédiatr 35: 383-6.
- Kriet M, Laktaoui A, Zrara S, Harmouchi N, Souhail H, et al. (2002) Esthésioneuroblastome olfactif de révélation ophtalmologique à propos d’une observation Journal Français d’Ophtalmologie 25: 632-35.
- Simon C, Toussaint B, Coffinet L (1997) Tumeurs malignes des cavités nasales et paranasales E.M.C, Paris, 20-405-A-10 (1997).
- Guerrier B, Chantrain G, Gallaux JP (1986) Olfactory esthesioneuroblastomas The ENT notebooks 9: 667.
- Thompson LD (2009) Olfactory neuroblastoma. Head Neck Pathol 3: 252-9.
- Bouziri M, Brahem D, Attia S, Ben Yahia S, Messaoud R, et al. (2008) Esthésioneuroblastome: à propos d’une observation Journal Français d’Ophtalmologie 31: 1-21.
- Hommadi A, Akhaddar A, Fehoume K, Chakir N, Jiddane M, et al. (2001) Apport de l’imagerie dans l’esthesioneuroblastome a propos d’un cas. Médecine du Maghreb 2001.
- brian Jason Schiro, Edward Joel Escott, Jonathan brad McHugh, Ricardo Luis Carrau (2008) Bone invasion by an esthesioneuroblastoma mimicking fibrous dysplasia, European J Radiology 65: 69–72.
- Zhang M, Zhou L, Wang DH, Huang WT, Wang Sy (2010) Diagnosis and management of esthesioneuroblastoma. ORL J Otorhinolaryngol Relat Spec 72: 113-8.
- Díez-Villalba R, González-Ruiz M, Izquierdo-Vázquez C, Sanz-Fernández R (2008) Debut oftalmológico de dos casos de estesioneuroblastoma Arch Soc Esp Oftalmol 83: 317-20.
- Kadish S, Goodman G, Wang SS (1976) Olfactory neuroblastoma: a clinical analysis of 17 cases. Cancer 37: 1471-576.
- Morita A, Ebersold MJ, Olsen KD (1993) Esthesioneuroblastoma: prognosis and management. Neurosurgery 32: 706-15.
- Dulguerov p, Allal AS, Calcaterra TC (2001) Esthesioneuroblastoma: a meta-analysis and review Lancet Oncol 2: 683–90.
- Thomas J Ow, Diana Bell, Michael E, Kupferman, Franco DeMonte, Ehab Y. Hanna, et al. (2013) Esthesioneuroblastoma.
- Iezzoni JC, Mills SE (2005) “Undifferentiated” small round cell tumors of the sinonasal tract: differentialdiagnosis update. Am J Clin Pathol 124: S110–21.
- Corneliu Toader, Marian Stroi, Andrei Kozma, Dorel Eugen Arsene (2018) Esthesioneuroblastoma: the complete picture – case report and review of the literature Rom J Morphol Embryol 59: 1211-8.
- Hyams VJ, Batsakis JG, Michaels L (1998) Tumors of the upper aerodigestive tract and ear. 2nd series ed. Washington: Armed Forces Institute of Pathology.
- Foote RL, Morita A, Ebersold MJ, O’fallon WM (1993) Esthesioneuroblastoma: the role of adjuvant radiation therapy Int Journal Radiation Oncology Biol Phys 27: 835-42.
- Bäck L , Oinas M , Pietarinen-Runtti P , Vuola J, Saat R, et al. (2011) The developing management of esthesioneuroblastoma: a single institution experience. European Archives of Otorhinolaryngol 1: 268.
- Gil-Carcedo E, Gil-Carcedo LM, Vallejo LA, Campos JM (2005) Esthesioneuroblastoma treatment Acta Otorrinolaringol Esp 56: 389-95.
- Turano S, Mastroianni C, Manfredi C, Viscomi C, Patitucci G, et al. (2010) Advanced adult esthesioneuroblastoma successfully treated with cisplatin and etoposide alternated with doxorubicin, J Neurooncol 98: 131–5
- Brian Fiani (2019) Esthesioneuroblastoma: A Comprehensive Review of Diagnosis, Management, and Current Treatment Options. Olfactory neuroblastoma review.
- Ozsahin M, Gruber G, Olszyk O, Matzinger O, Zouhair A, et al. (2010) Outcome and prognostic factors in olfactory neuroblastoma: a rare cancer network study. Int J Radiat Oncol Biol Phys 78: 992-7.
- Saade RE, Hanna EY, Bell D (2015) Prognosis and biology in esthesioneuroblastoma: the emerging role of Hyams grading system. Curr Oncol Rep 17: 1–5.
- Schwartz JS, Palmer JN, Adappa ND (2016) Contemporary management of esthesioneuroblastoma. Curr Opin Otolaryngol Head Neck Surgery 24: 63–9.
- Suriano M, De VincentiisM, Colli A, Benfari G, Mascelli A, Gallo A (2007) Endoscopic treatment of esthesioneuroblastoma: a minimally invasive approach combined with radiation therapy. Otolaryngol Head Neck Surg136: 104–7.
- Loy AH, Reibel JF, Read PW, Thomas CY, Newman SA, (2006) Esthesioneuroblastoma: continued follow-up of a single institution’s experience. Arch Otolaryngol Head Neck Surg 132: 134-8.
- Lee D Cranmer, Bonny Chau (2019) MPHChemotherapy in Esthesioneuroblastoma/Olfactory Neuroblastoma An Analysis of the Surveillance Epidemiology and End Results (SEER). Ame J Clinical Oncology.
- Su SY, Bell D, Ferrarotto R (2017) Outcomes for olfactory neuroblastoma treated with induction chemotherapy. Head Neck 39: 1671–9.
- Kane AJ, Sughrue ME, Rutkowski MJ (2010) Post treatment prognosis of patients with esthesioneuroblastoma. J Neurosurg113: 340-51.
- Alotaibi HA, Priola SM, Bernat AL (2019) Esthesioneuroblastoma: summary of single-center experiences with focus on adjuvant therapy and overall survival Cureus 11: e4897.
- Alvarez I, Caminero (1995) Pronostic factors in paranasal sinus cancer Ame J Otolayngol 16: 109-114.

Tables at a glance
Figures at a glance