Consequences of the Covid-19 Pandemic in the Organization of the Obstetric Unit and Adaptation to the New Situation
Received Date: August 09, 2020 Accepted Date: August 25, 2020 Published Date: August 28, 2020
doi: 10.17303/jwhg.2020.7.401
Citation:Noguero Meseguer M. Rosario (2020) Consequences of the Covid-19 Pandemic in the Organization of the Obstetric Unit and Adaptation to the New Situation.J Womens Health Gyn 7: 1-11.
Abstract
Introduction: COVID 19 pandemic is causing several changes in the organization of obstetric units, due to the lack of space and the need of avoiding new infections among professionals and patients
Objective: To describe the differences in the obstetric unit practice caused by the COVID pandemic.
Material and Methods: We performed a retrospective study comparing 2 groups of obstetrics patients: “2020 COVID pandemic” group which included patients admitted in the obstetric unit of Hospital Rey Juan Carlos, in labor or with premature rupture of membranes (PRM) from 09/03/2020 to 17/04/2020, and “2019” group which included patients admitted for the same reasons during the same period in 2019.
Results: We included 200 patients in the “2020 COVID pandemic” group and 219 in the “2019” group. We found that active management of (PRM) increased significantly in the “2020 covid pandemic” group compared to “2019” group. (71.8% versus 11.6%) (p = 0,0001). The number of cesarean sections was also significantly increased (16% vs 13%) (p = 0,02), as well as the instrumental delivery (13% versus 8%) (p = 0,02) and episiotomies (15% vs 7.5%) (p = 0,001). Despite this, we found no significant increase in the incidence of intrapartum fever, postpartum complications or in the number of admissions to the neonatal unit. The average hospital stay decreased significantly in 2020 (1.93 ± 0.74 versus 2.77 ±,640) (p = 0,0001), because of early obstetric discharges. The statistical significance p-value was defined as p < 0,05. Among the pregnant women included in the “2020 COVID Pandemic” group, three infected with 2019-nCov were treated following the current protocol
Conclusions: Our obstetric practice has been deeply modified during Covid19 pandemic, with an increase in more active management and a decrease in the average hospital stay
Keywords: COVID 19; Premature Rupture of Membranes; Labor Induction; Rate of Cesarean Section; Instrumental delivery; Episiotomie.
Introduction
COVID-19 is an emerging disease with a rapid increase in cases and deaths since it was first detected in Wuhan, China, in December 2019. The infectious agent has been identified as SARS-CoV-2. Even now, it continues to expand in all countries around the world [1].
The COVID-19 pandemic has caused numerous changes in the operation of hospitals, such as the obstetric unit. The need to enable spaces and rooms (ICU and hospitalization) for COVID-19-positive patients has led to the reduction of the dimensions of units such as delivery rooms, a situation that in some centers has even led to the complete cessation of any obstetrics activity
There is limited information on the effects of the coronavirus in pregnant women and the newborn [2, 3]. Likewise, there is not much literature on the higher infectious risk or higher susceptibility for the SARS-CoV-2 infection in pregnant women, or the development of more severe pneumonia, or the impact in the functioning of the delivery rooms. However, at the time of delivery, extreme attention must be given to prevention, diagnosis, and management, and in this regard, informational guidelines have been issued in recent months for the care of women during their admission to give birth [4]. The reasons for our work would focus on the application of some of these guidelines in our obstetrics field, and the changes made in the operation of the Maternity, during the period of the greatest number of COVID-19 cases in Spain, which began on March 9th, 2020.
Objectives
The objective of this work is to analyze the changes taken place in the healthcare practice, and the effects or complications on pregnant women, caused by the COVID-19 pandemic in the delivery room of the Rey Juan Carlos Hospital (Madrid, Spain), coinciding with the period of the largest number of people affected in Spain. We compared this practice with the maternity care practice during a similar period of time in 2019.
Methodology
The current study is a retrospective analysis of the modifications in the healthcare practice, and the effects or complications on pregnant women, comparing two groups of pregnant women who attended the obstetric unit of our hospital at two-time points: The first group, called “2020 COVID Pandemic”, made up of pregnant women we attended to from March 9th to April 17th, 2020 (the most critical period of the pandemic), and the second group called “2019”, made up of pregnant women attended during the same period of 2019. We also carried out a descriptive analysis of the evolution of the 3 pregnant women diagnosed with coronavirus at our unit.
The information was obtained by reviewing the electronic medical record. Inclusion criteria were: pregnant women with a gestational age greater than 32 weeks, who were admitted with premature rupture of membranes (PROM), labor in progress, labor induction or scheduled cesarean section.
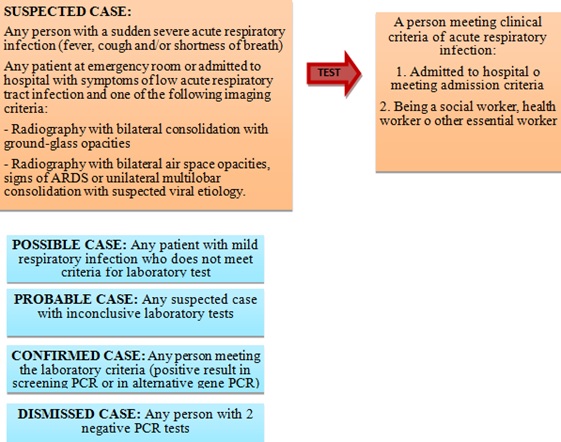
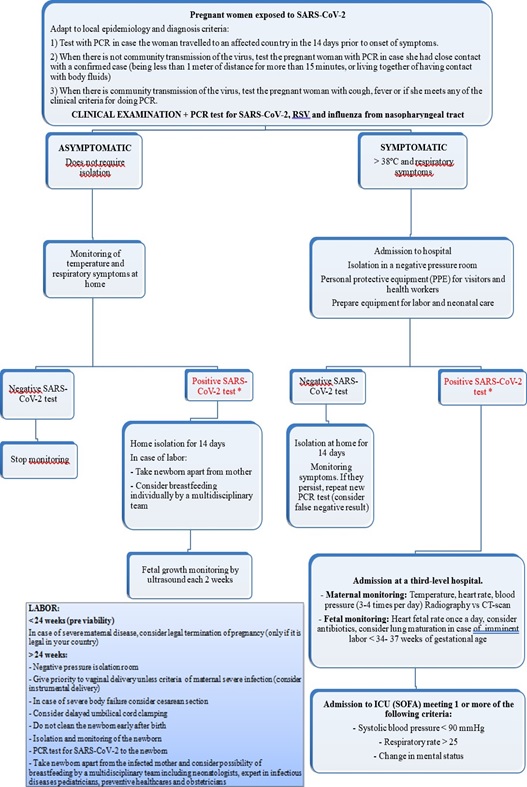
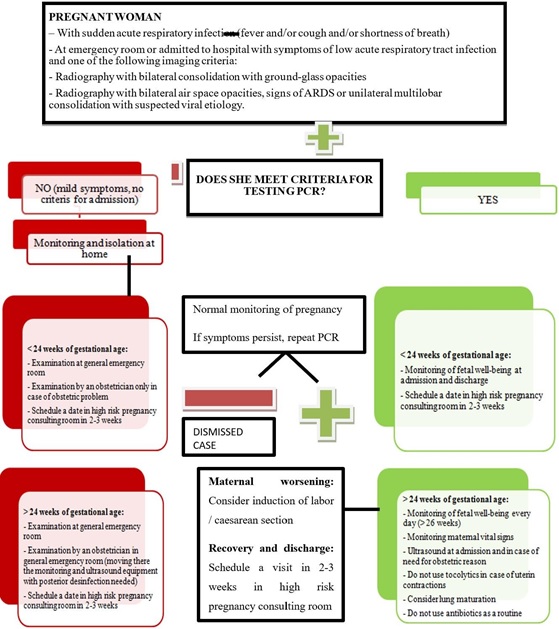
In the case of pregnant women positive for coronavirus or suspicion of infection, the indications established by the Spanish Ministry of Health (Illustration 1) and the procedure for childbirth care that is reflected in Illustration 2 and 3 were applied [5].
This study was carried out in accordance with the protocol and with the guidelines of Good Clinical Practice, as described in:
- The harmonized standards of ICH E6 of Good Clinical Practice of 1996. - The 14/2007 Law on Biomedical Research. - The 2001/20/EC Directive. - The update of the Declaration of Helsinki and the modifications related to medical research in humans. - -It is a retrospective study, the request for informed consent was not required, and preserving confidentiality and not re-identifying the data was left to the researchers.
The researchers agreed, by signing the protocol, to follow the instructions and procedures described in it and, therefore, to comply with the principles of Good Clinical Practice on which it is based. Once the protocol was signed, it should not be modified without the written agreement of the principal investigator and with the consent of the Ethics Committee.
Ethics Committee
Before the implementation of this study, the protocol and its annexes were reviewed by the Ethics and Drug Research Committee (CEIm) of the IIS-FJD Research Institute
Confidentiality
The treatment, communication, and transfer of personal data of all participating subjects followed the current Spanish laws and regulation
Economic Report
This study was an independent initiative of a group of researchers led by the Obstetrics and Gynecology Service of the Rey Juan Carlos University Hospital and did not require any funds to be carried out.
Statistical Analysis
The qualitative variables are expressed as percentages and the quantitative variables as mean and standard deviation. The inter-group comparison of the quantitative variables was performed using the parametric test of the Student t. The inter-group comparison of categorical variables was performed using the Chi-square test and Fisher’s exact test. The level of significance was defined as a value of p < 0.05. For statistical analysis, SPSS for Windows version 15.0 IBM Chicago USA was used.
Results
At our hospital, assistance during delivery is usually carried out in the Obstetric Unit, which includes six labor and delivery rooms, two rooms for maternal and fetal monitoring, one room for ambulatory care, and two examination rooms for emergency care. The unit has a waiting room for patients and an operating room available in the surgical area attached to the obstetric unit
Under normal conditions, after the delivery or the cesarean section procedure, patients are transferred to the maternity ward, and discharge is arranged after two or three days (depending on whether it was a vaginal birth or cesarean section), a stay conditioned by the metabolic tests of the newborn.
As the number of admissions for COVID-positive patients increased, all hospitalization floors were re-converted and intended for Coronavirus patients. In this situation, the delivery room was transformed to assume the postpartum hospitalization in the same location. A labor room was reserved for COVID-positive pregnant women, following the recommended requirements for their isolation and ventilation.
During the studied period of 2020, no PCR determinations or serological tests for COVID-19 were performed on any of the pregnant women who were admitted because of labor, PROM or scheduled cesarean section, unless they were symptomatic and met the indications established by the Spanish Ministry of Health (Illustration 1).
The early discharge was applied 24 hours after a eutocic delivery and 48 hours in the case of the cesarean section. Mothers and newborns were provided with an appointment to carry out the metabolic and otoacoustic emissions tests in the same Obstetric Unit 24 hours after discharge.
The group “2020 COVID Pandemic” was made up of 200 women, and the group “2019” of 219. All of them were admitted to the obstetric unit of the Rey Juan Carlos Hospital.
Socio-Demographic Characteristics of the pregnant women included in the study
The mean maternal age was 32.3 ± 5.6 years in the “2020 COVID Pandemic” cohort and 32.4 ± 5.3 years in the “2019” group, a difference that was not statistically significant (p= 0.2). The mean gestational age was 39.2 ± 1.9 weeks in the 2020 group and 39.1 ± 2.9 weeks in the 2019 group (p = 0.7). There was 5% prematurity (< 37 weeks) in the 2020 group and 3.5% in the 2019 group, without statistical differences. The gestational age in all cases was over 34 weeks.
Changes in obstetric care practice and effects on pregnant women (Table 1)
There were no significant differences in the number of inductions in the “2020 COVID Pandemic” group (33.1% vs. 44%) (p = 0.06), but the guidelines for administration of cervical prostaglandins (dinoprostone and misoprostol) were shortened, combined with an earlier and the more frequent application of amniorrhexis and the use of oxytocin (60.2% vs. 33.7%) (p = 0.01).
The way of proceeding when treating premature rupture of membranes (PROM) was affected, with a significant increase in active management in the “2020 COVID Pandemic” group (71.8% vs. 11.6%) (p = 0.0001), with much more frequent use of oxytocin due to the need to shorten times.
The pandemic situation notably influenced the number of cesarean sections, showing a significant increase of 5 percentage points compared to the same period of the previous year (18% in 2020 vs. 13% in 2019) (p = 0.02). The increase took place at the expense of the indications for “concerns over fetal well-being” and “failure to progress”. However, there were no more cesarean sections because of “failed induction” (because of PROM or other reasons).
Compliance with the cesarean section standard, which consists in applying certain rules to the indication of cesarean sections with an ensuing assessment by an obstetric team, fell to 82.8% in the “2020 COVID Pandemic” group (it was 100 % in the 2019 group), mainly at the expense of those under an indication of “failure to progress”.
Despite the increase in the number of surgical deliveries and the pandemic situation, the humanization protocol for cesarean sections, which allows family reunion immediately after surgery, was followed in 75% of the cases (79% in 2019, p = 0.8).
The number of instrumental deliveries increased significantly, going from 8% to 13.4% in the “2020 COVID Pandemic” group (p = 0.02), mainly using Kiwi vacuum cups and Kielland’s forceps to shorten the expulsion period.
The number of episiotomies doubled compared to the previous year, to speed up the expulsion period of labor and due to the greater number of instrumental deliveries (15% vs. 7.4%, p = 0.001), a circumstance that did not increase the number of perineal tears, which was maintained in similar figures in both groups of pregnant women.
During the analyzed period, spinal anesthesia was offered as usual, to 82.5% of pregnant women (p = 0.8), although we recorded a drastic reduction in the use of Kalinox (from 12.9% to 1.5 %, p = 0.0001), because of its contraindication due to the risk of coronavirus transmission.
The incidence of pregnant women with intrapartum fever was higher in the “2020 COVID Pandemic” group than in the “2019” group but without statistical significance (p= 0.7).
The average length of hospital stay during the COVID-19 pandemic was significantly reduced because of the generalization of early discharges; thus, it was 1.9 ± 0.7 days in the “2020 COVID Pandemic” group, compared to 2.8 ± 2.85 in the “2019” group (p = 0.0001).
The more frequent puerperal complications included uterine atony, postpartum hemorrhage, and postpartum fever. There were no significant differences in the comparison of both groups (p = 0.9). Breastfeeding and “skin to skin” were carried out as usual in the “2020 COVID Pandemic” group, without significant differences from the previous year (p = 0.9 and p = 1, respectively).
The number of newborns admitted to the Neonatal Service decreased (there were 10 in the 2020 group and 15 in the 2019 group). The rest remained with their mothers after delivery. The reasons for admission were: respiratory distress, hypoglycemia, suspicion of COVID-19 (1 in 2020), prematurity, and observation.
In our study, we reported a series of three cases of pregnant women diagnosed with COVID-19 infection (all of them PCR-confirmed from a nasopharyngeal exudate, performed because they presented symptoms compatible with this condition); the reason for termination of pregnancy in these cases was the diagnosis of COVID-19 infection in a pregnant woman at term (with less than 10 days between the onset of symptoms and delivery in all three cases). The predominant route of delivery was cesarean section (2/3 cases), performed under indications other than the infectious symptoms (“failure to progress” and rejection of vaginal delivery in a patient with a previous cesarean section). No newborn required resuscitation or hospitalization, and neonatal transmission was not observed, with all babies presenting two negative PCRs from nasopharyngeal exudate at birth (separated by 24h). No serological study, amniotic fluid study or umbilical cord blood study was performed on the babies.
Regarding the maternal results in our series, the evolution of the SARS-CoV-2 infection was favorable (2 cases of pneumonia without any respiratory failure associated and one case who showed respiratory symptoms with a normal chest X-ray), with none of the women requiring ICU admission.
Discussion
The coronavirus pandemic has had a major impact on the operation of the various hospital structures, as well as on the assistance provided in the delivery rooms and maternal hospitalization facilities. In the application and development of all these changes, we rely on the updated recommendations that emerge in the literature, specifically those presented by the group of Boelig RC et al. [4].
To study the repercussion of the COVID-19 pandemic in our hospital, we analyzed two groups: one group of pregnant women who gave birth in our maternity ward in the time period of the pandemic between March 9 and April 17 in the year 2020 and another group of pregnant women who gave birth in our maternity ward during a similar period of 2019. These two groups were comparable in terms of maternal age and gestational age at admission.
In the “2020 COVID Pandemic” group, active management of PROM was significantly increased, with the aim of minimizing the length of hospital stay and reducing the risk of contagion by coronavirus as much as possible. This measure increased the use of oxytocin; however, it was not accompanied by an increase in the indication for cesarean section due to failure of induction because of PROM. In the current bibliography, we did not find references related to the management of PROM in pregnant women not infected with Coronavirus.
In the current literature, there is no clear evidence in favor of active management compared to expectant management of PROM in pregnancies at term, although the reduction in delivery time, the chorioamnionitis rate, and the number of admissions in neonatal units have been described [6]. Scientific societies such as ACOG [7] accept both active management and expectant management at term. In our hospital, we offer both options, with an expected period of 12 hours, as long as the amniotic fluid is clear, maternal infection is ruled out and fetal well-being is verified.
The behavior in labor inductions was also modified, prioritizing artificial amniorrhexis after a favorable examination of the uterine cervix (Bishop index) and the use of oxytocin rather than the use of cervical prostaglandins. In those patients who received prostaglandins, cervical maturation times were also shortened. The published bibliography ratifies that these two induction methods are the most effective in order to achieve vaginal delivery within the following 24 hours, opting for one or the other depending on the obstetric examination [8, 9, 10].
In the “2020 COVID Pandemic” group, the number of cesarean sections increased by 5 percentage points, mainly due to indications of “failure to progress” and “concerns over fetal well-being”. Our usual obstetric behavior, outside of the pandemic period, is governed by the Standardized Cesarean protocol, chosen in 2014 by the Spanish Ministry of Health as “good obstetric practice” [11] and which entails little interventionist attention to childbirth. Basically, the protocol marks the application of some established standards for the indication of cesarean sections, with an ensuing review by a team of obstetricians that assesses whether the performance followed the standard. Thanks to this protocol, we usually register a very low C-section rate in our Center, which normally ranges between 12-13% outside the pandemic situation.
The application of the standard for cesarean sections [12] was deeply affected by the COVID-19 pandemic, particularly in the C-sections performed due to “failure to progress”, in a scenario in which this methodology was difficult to implement, based on the Harper and Zhang curves [13,14] which allow adjusting the times of labor progression in those cases of spontaneous onset of labor as well as in induced and stimulated deliveries. In the C-sections performed due to “concerns over fetal well- being”, the standard was followed in all cases.
The higher obstetric interventionism was also evident in the significant increase in instrumental delivery and in the number of episiotomies. Again, the need to reduce labor times led to a change in the way of proceeding in the last phase of labor or “expulsive period” after complete dilation, with an approximate duration of 1 hour in multiparous and 2 hours in nulliparous women. Thus, directed pushing was prioritized over passive fetal descent, as we had been doing regularly following the literature [15].
Current clinical guidelines and the literature published so far advocate for shortening the expulsion period, as it represents the moment of highest risk of transmission of SARSCoV-2, due to the expulsion of more respiratory droplets (even when the patient is carrying a surgical mask), and of greatest maternal exhaustion. This is why the increase in the number of instrumental deliveries and episiotomies would be justified [16,17].
The pandemic context did not modify the administration of spinal anesthesia, which continued to be used in all pregnant women who requested it and in a similar proportion than other times, its widespread use recommended given the fact that it decreases the possibility of general anesthesia in the case of an obstetric emergency. It is worth noting the almost total reduction in the use of Kalinox, because of the greater risk of coronavirus contagion that could derive from nebulization [18].
The pandemic state allowed us to continue with our protocol of humanization of cesarean sections, which preserves the family unit (father-mother-newborn), during the immediate postoperative period.
Similarly, breastfeeding was not affected and “skinto-skin” contact with the baby after birth was encouraged. No greater number of puerperal complications occurred.
Early discharge shortened the average stay and greatly modified the role of the Neonatal Service since many women were discharged from the hospital within the first 24 hours after delivery and came back the following day for the baby’s checkup and the performing of metabolic tests. However, this change in behavior was not accompanied by a greater number of admissions and readmissions in the Neonatal Service, compared to the previous year. There was only one case of dehydration in a newborn after early discharge, which evolved optimally.
In our study, we report a series of three cases of pregnant women diagnosed with coronavirus infection, in which the predominant way of delivery was a cesarean section (2/3 cases), for reasons not related to the infection, a finding that coincides with the cases published, although the reason for performing the cesarean section is not specified in most of the series [2,3]. The three women had a good postpartum evolution, a finding that matches the series published by Breslin N et al. [19].
None of the births was premature, in contrast with other published series in which the prematurity rate reached 47%. The reason for this discrepancy could reside in the small size of our sample [20].
Limitations
There are some limitations in our study. Firstly, the small sample size and the profile of the Obstetric Unit (delivery room) do not allow us to make conclusions that can be extrapolated to other institutions.
Secondly, during the studied period of 2020, no PCR test (from a nasopharyngeal exudate) or serological testing for COVID-19 were performed on any of the pregnant women who were admitted with labor, PROM or scheduled cesarean section, unless they were symptomatic and met the indications established by the Spanish Ministry of Health. This fact may limit the conclusions about the impact of Coronavirus infection on the obstetrics results.
Conclusions
Our obstetric practice has been deeply modified during the Covid19 pandemic, with an increase in more active management in treating PROM, much more frequent use of oxytocin due to the need to shorten labor times, a significant increase in the rate of caesarian sections and instrumental deliveries.
As a consequence, the average length of hospital stay during the COVID-19 pandemic was significantly reduced because of the generalization of early discharges.
However, these changes in behavior were not accompanied by a greater number of admissions and readmissions in the Neonatal Service, or by postpartum maternal complications.
Acknowledgments
We would like to express our gratitude towards the midwives, clinical assistants, and all our colleagues of the Department of Obstetrics and Gynecology for their kind cooperation and encouragement which helped us in developing the project.
- (2020) COVID-19 situation reports.
- Zhu H, Wang L, Fang C, Peng S, Zhang L, et al. (2020) Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 9: 51-60.
- Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. (2020) Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet Lond Engl. 395: 809-815.
- Boelig RC, Manuck T, Oliver EA, Di Mascio D, Saccone G, Bellussi F, et al. (2020) Labor and Delivery Guidance for COVID-19. Am J Obstet Gynecol MFM 100110.
- Martinez-Portilla RJ, Goncé A, Hawkins-Villarreal A, Figueras F (2020) A Spanish- translated clinical algorithm for management of suspected SARS-CoV-2 infection in pregnant women. Lancet Infect Dis
- Bond DM, Middleton P, Levett KM, van der Ham DP, Crowther CA, Buchanan SL, et al. (2017) Planned early birth versus expectant management for women with preterm prelabour rupture of membranes prior to 37 weeks’ gestation for improving pregnancy outcome. Cochrane Database Syst Rev
- (2020) Prelabor Rupture of Membranes: ACOG Practice Bulletin, Number 217. Obstet Gynecol. 135: e80-97.
- Saá L, Ríos MD, Meseguer M (2017) Low-Dose Misoprostol versus Vaginal-Insert Dinoprostone for At-Term Labor Induction: A Prospective Cohort Study. Open J Obstet Gynecol 7: 824- 34.
- Kolkman DGE, Verhoeven CJM, Brinkhorst SJ, van der Post JAM, et al. (2013)The Bishop score as a predictor of labor induction success: a systematic review. Am J Perinatol. septiembre de 30: 625-630.
- Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Medley N, Dias S, et al. (2016) Methods to induce labor: a systematic review, network meta-analysis and cost-effectiveness analysis. BJOG Int J Obstet Gynaecol 1462-1470.
- (2014) Ministry of Health, Consumption, and Social Welfare - Institutional Organization of Good Practices in the Strategy for Childbirth Care and Reproductive Health of the SNS.
- Calvo Pérez A, Campillo Artero C, Roig Julià C, Cabeza Vengoechea PJ (2019) A multifaceted model to improve the adequacy of caesarean section indications. Prog Obstet Ginecol.
- Harper LM, Caughey AB, Odibo AO, Roehl KA, et al. (2012) Normal progress of induced labor. Obstet Gynecol 119: 1113- 1118.
- Zhang J, Troendle J, Mikolajczyk R, Sundaram R, et al. (2010) The natural history of the normal first stage of labor. Obstet Gynecol 115: 705-710
- Cahill AG, Srinivas SK, Tita ATN, Caughey AB, Richter HE, Gregory WT, et al. (2018) Effect of Immediate vs Delayed Pushing on Rates of Spontaneous Vaginal Delivery Among Nulliparous Women Receiving Neuraxial Analgesia: A Randomized Clinical Trial. JAMA 320:1444-1454.
- Yang H, Wang C, Poon LC (2020) Novel coronavirus infection and pregnancy. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol 55: 435-437.
- (2020) ISUOG Interim Guidance on 2019 Novel Coronavirus Infection During Pregnancy and the Puerperium.
- soapwpadmin. Interim Considerations for Obstetric Anesthesia Care Related to COVID19.
- Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, et al. (2020) COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 100118.
- Mullins E, Evans D, Viner RM, O’Brien P, Morris E (2020) Coronavirus in pregnancy and delivery: a rapid review. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol.

Tables at a glance