The Co-Analgesic Efficacy of Preoperative Single Dose Gabapentin after Surgical Removal of Lower Third Molars
Received Date: December 10, 2021 Accepted Date: January 10, 2022 Published Date: January 12, 2022
doi: 10.17303/jdoh.2022.9.101
Citation:Hanna Frelich-Truchel (2022) The Co-Analgesic Efficacy of Preoperative Single Dose Gabapentin after Surgical Removal of Lower Third Molars. J Dent Oral Health 9: 1-10.
Abstract
A procedure of the surgical removal of impacted lower third molars is the most frequently performed procedure by dentists. Simultaneously, it causes the most fear and anxiety for patients. Patients are afraid of intraoperative pain and complications that may occur following the procedure. Despite the development of surgical methods and pharmacology, pain remains an unsolved issue. Gabapentin has been used as a coanalgesic in surgery for many years, however, there is no research indicating the use of gabapentin for dental pain.
The objective of this study was to assess the effectiveness of gabapentin in relieving pain after dental surgery and its impact on the patients’ intake of painkillers.
Materials and methods:The study included 47 patients who underwent surgical extraction of impacted third molars at the Specialist Dental Center A.H. Frelich in Żory Poland. Patients were divided into two groups, a study group and a control group, to which they were randomly assigned. Randomization was done by flipping a coin. The study group in which the patients received gabapentin an hour before the procedure and the control group in which patients did not take gabapentin. After surgery, patients took paracetamol and diclofenac as needed. The pain level was assessed with the help of the NRS scale at 0.5, 2, 6, 12, 24, 48 hours after the procedure.
Results:There was no significant difference noted in the pain intensity in the compared groups. There was also no difference in the number of painkillers taken by the patients in the study and control groups. There were statistically significant differences in the average pain intensity in the analyzed time intervals and the associated lower demand for painkillers in the 0.5-2h time interval.
Conclusion:A single dose of gabapentin before the procedure does not reduce pain or the need for analgesics in patients undergoing extraction of lower third molars.
Keywords:Gabapentin; Extraction of Impacted Molars; Multimodal Therapy; Acute Pain Relief
Introduction
Extraction of third molars, commonly called wisdom teeth, is one of the most common dental surgical procedures. The procedure poses difficulty due to the uneasy access to this area and the frequent need to remove hard bone. Patients often develop postoperative edema, pain or trismus. Studies have shown that about 50-70% [1] of patients experience moderate to severe pain after the procedure. Despite the introduction of new pharmacological agents and the development of improved techniques, the problem of postoperative pain remains underestimated and postoperative analgesia is still insufficiently controlled. The most severe pain occurs approximately 3-5 hours after dental procedure and may persist for up to 2-3 days. [1]
In the absence of acute inflammation, the procedure is painless as it is performed under local anaesthesia. Articaine, which, due to its structure, undergoes a two-stage breakdown both in the plasma and in the liver, is one of the most frequently used dental anaesthetics. It shows good bone penetration and low toxicity. When combined with epinephrine, its anaesthetic effect lasts 2-7 hours, which allows for a painless initial period after the procedure.
Pain after tooth extraction develops as a multistage process. During the procedure, inflammatory mediators such as for example histamine, leukotrienes, prostaglandins, cytokines, and bradykinins are released. These substances cause hyperalgesia in the treated site and adjacent tissues. The pain stimulus from afferent neurons is conducted through the spinal cord to higher brain centres, where it is modulated by, among others, endogenous opioids, noradrenaline, and 5-hydroxytryptamine (serotonin, 5-HT). The currently recommended multimodal analgesia should control pain at every stage of its development, from generation through conduction to processing and modulation [2]. This way, it is more effective.
Non-steroidal anti-inflammatory drugs (NSAIDs) and selective COX-2 inhibitors have an impact on pain stimulus transduction; regional blocks affect conduction; opioids, clonidine, selective COX-2 inhibitors, ketamine, and gabapentin affect modulation; opioids, clonidine, ketamine, gabapentin modulate perception, while antidepressants have an impact on the CNS response. The current pharmacotherapy of postoperative pain involves the use of analgesics with the so-called co-analgesics such as lidocaine, NMDA receptor antagonists (ketamine, magnesium sulfate), corticosteroids, calcium channel inhibitors (gabapentin,pregabalin) or α2 adrenergic receptor agonists (clonidine, dexmedetomidine) [2]. In addition to the standard pharmacological agents, we may find attempts to administer non-pharmacological agents such as ozone, laser therapy, cryotherapy [3].
Gabapentinoids are a group of agents used to treat epilepsy and neuropathic pain. They are also a promising alternative in the adjunctive therapy of postoperative pain. They block voltage-gated ion channels for calcium ions in the structures of the nervous system. Their use reduces the release of pronociceptive neurotransmitters. Clinical trials on acute pain have shown the usefulness of these agents in the treatment of acute neuropathic pain, which allows for the reduction of opioid doses and, consequently, their adverse effects. Long-term observations showed lower rates of postoperative chronic pain [2, 4].
Gabapentin is a recommended and proven co-analgetic for the treatment of postoperative pain in many surgical interventions, but there are no scientific studies on its co-analgesic effects during an extraction of mandibular third molars. The aim of the study was to assess the effect of a single dose of gabapentin before surgical extraction of impacted lower third molars on pain reduction and the need for postoperative analgesics.
Materials and Methods
Patients with ASA (The American Society of Anesthesiologists) I-II classification aged 18-50 years with indications for mandibular third molar extraction were included in the study. Patients treated for epilepsy, allergic to any substances used in the study, those on chronic analgesic therapy, as well as pregnant and breastfeeding women were excluded from the study. This was a prospective, cohort, randomised study. The study was approved by the Bioethics Committee of the Silesian Medical Chamber (Resolution No. 2/2018). It was conducted at the Specialist Dental Center in Żory. Informed, written consent was obtained from each participant. Surgical extraction of third molars was performed in patients randomly assigned to two groups. Patients in the study group received a single dose of 600 mg of gabapentin (Gabapentin Teva, Poland) an hour before the procedure, and then underwent the extraction exactly the same way as the control group. Bone preparation was performed with a water-cooled bur.
The study was conducted in 47 patients, of which 24 administered gabapentin before the procedure and 23 were not given this drug. There were 15 men and 32 women in the study group. The results are presented as absolute numbers and percentages. A p-value of <0.05 was considered significant.
Conduction anaesthesia was administered in the area of the inferior alveolar and lingual nerves, and the buccal nerve was infiltrated with a dose of 80 mg of articaine with 0.024 mg of norepinephrine. ( Articaini hydrochloridum + Epinephrini hydrochloridum 40mg + 0,012mg, Germany). Postoperatively, the patients received 0.5-1g of paracetamol (Paracetamol, Aflofarm Poland) every 6 hours, 25-50 mg of diclofenac (Diclac 50, Sandoz Poland) every 8 hours and tramadol (Tramal, STADA Germany) at a dose of 25-50 mg every 4-6 hours if needed. After the procedure, the patients received a form to report the severity of pain according to the NRS and the need for analgesics at different time points after the procedure (30 min, 2hrs, 6 hrs, 12 hrs, 24 hrs, 48 hrs). This scale contains 11 degrees of pain severity. The patient is asked to describe how severe the pain is, indicating the appropriate number, where 0 means “no pain” and 10 means “worst pain I can imagine”.
Statistical analysis was performed using StatSoft, Inc. STATISTICA (data analysis software system), version 12. Spearman’s rank correlation coefficient was used to determine the relationship between variables. Comparison of numbers in the study groups was performed using Pearson’s Chi2 test.
Results
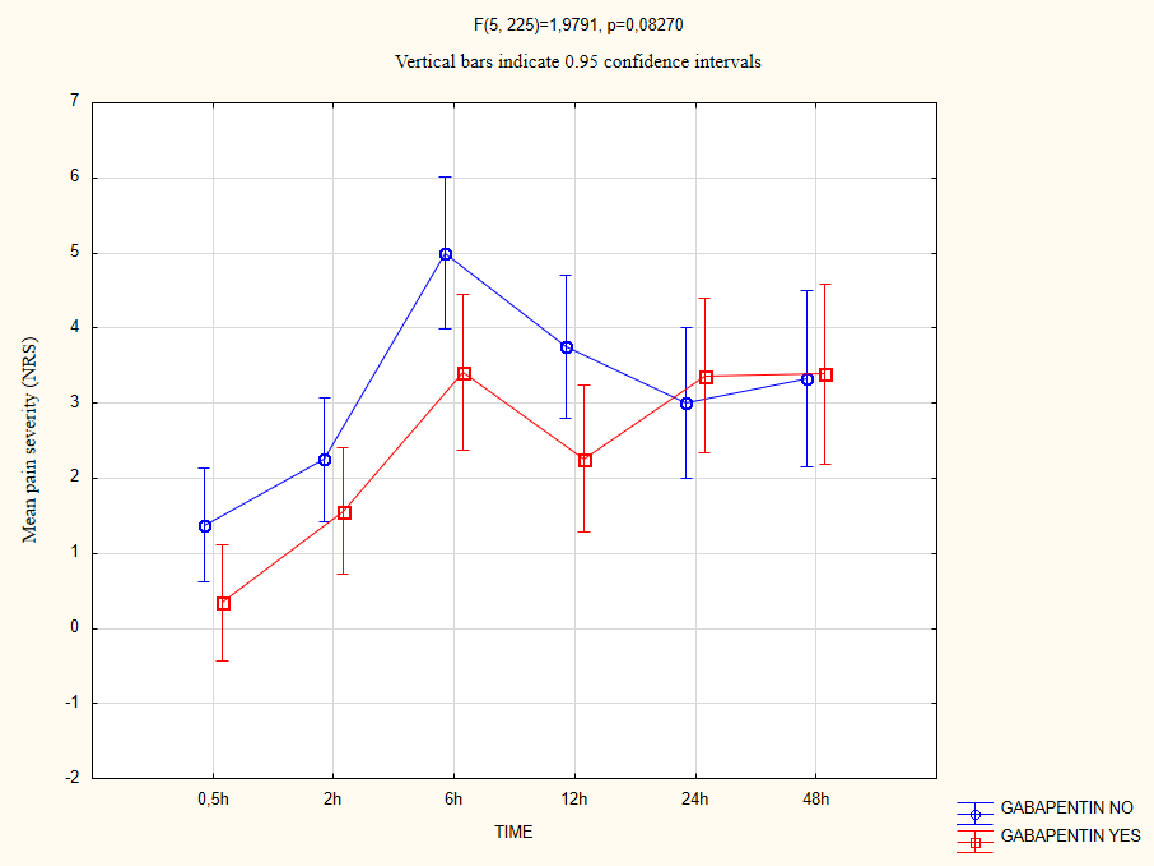
All patients followed up. The mean pain severity (NRS) reported by patients before extraction was 2.4 in the study group and 3.1 in the control group. The difference was not statistically significant. We compared the mean pain intensity in both groups at selected time points. We found higher mean pain intensity in the control group in the time interval between 0.5 hrs and 24 hrs, which then decreased between 24hrs to 48hrs (p=0.827) (Figure 1).
We then assessed the impact of gabapentin on the need for analgesics. Three patients in the study group needed no additional medications, and all patients in the control group used additional analgesics. Both in the control group and the study group, 11 patients used only one medication, while both drugs were used by 13 and 9 patients, respectively. There was no significant difference in the number of analgesics administered between the gabapentin group and controls (Table 1).
We investigated the mean use of analgesics in different time intervals and found a significant difference in the mean amount of these agents depending on the time elapsed since the procedure. The greatest difference in the need for medications was found between the baseline measurement (0.5 hrs) and 6-48 hrs after the procedure. The lowest drug use was observed 0.5-2 hours after the procedure. The highest use of analgesics was recorded at 48 hours after third molar extraction. We found no significant difference in the mean consumption of paracetamol and diclofenac in the gabapentin group and patients who did not receive this agent (p<0.05) (Figure 2).
We also verified whether gender influenced the perception of postoperative pain. There was no significant difference in the mean pain severity between women and men in the analysed time intervals (Figure 3).
Discussion
Surgical extraction of the third molar is a source of increased anxiety for the patient. Patients are most often concerned about the perioperative pain, which is acute and limited to the treated area. However, adjacent teeth and anatomical structures may be also involved. The inflammatory component and mechanical trauma play an important role in the genesis of pain [5]. The perception and modulation of pain stimuli are influenced by gabapentin, which is used as a co-analgesic in acute and chronic pain. We can find descriptions of its use in e.g. thoracotomy, thoracoscopy, mastectomy and many orthopedic procedures [6]. Hah, et al. [6] investigated the efficacy of gabapentin in reducing postoperative pain and opioid use in the above-mentioned surgeries. They showed that although gabapentin did not reduce postoperative pain, it reduced the need for opioid use. Dirks, et al. [7,8] also investigated the efficacy of gabapentin in reducing morphine intake after hysterectomy and mastectomy. Gabapentin reduced the total need for morphine in both cases. However, not all studies on gabapentin and its co-analgesic action prove its efficacy. Kinney, et al. [9] investigated the efficacy of gabapentin in multimodal therapy in patients undergoing elective thoracotomy. However, they did not show any reduction in pain severity or lower opioid consumption in patients receiving a single preoperative dose of gabapentin [9].
In our study, no statistically significant difference was found in pain severity or the need for analgesics between the patients in the study group and controls. However, the pain severity tended to drop (p = 0.083) in the first 12 hours after the procedure in patients who received gabapentin. The study showed a higher mean pain intensity in the control group in the time interval between 0.5 hrs and 24 hrs, which then decreased in the time interval 24 hrs -48 hrs. This may be related to the duration of gabapentin action, which is 8-12 hours [10].
The study showed that a single application of gabapentin before the procedure does not reduce pain or the need for analgesics in patients undergoing extraction of lower third molars. In our study, a statistically significant lower pain sensation was found in the time interval of 0.5-2 hour. Such results may indiecate properly performed local anaesthesia, which, by inhibiting the transmission of pain, ensures absence of or reduced pain. The stimulus does not reach the central nervous system, which excludes the analgesic mechanism of gabapentin.
Many studies report that gender is one of the factors influencing the perception of pain. Experimental data show that both the different modulation of the endogenous opioid system and sex hormones are factors influencing pain in women and men [11]. Our study showed no statistically significant difference in pain perception depending on gender. This may be related to the relatively small size of the group we examined.
Conflicts of Interest Statement
The authors declares that there is no conflict of interest.
- Raiesian S, Khani M, Khiabani K, Hemmati E, Pouretezad M (2017) Assessment of Low-Level Laser Therapy Effects After Extraction of Impacted Lower Third Molar Surgery. J Lasers Med Sci 8: 42-5.
- Wordliczek J, Zajączkowska R, Dziki A (2019) Postoperative pain relief in general surgery - recommendations of the Association of Polish Surgeons, Polish Society of Anaesthesiology and Intensive Therapy, Polish Association for the Study of Pain and Polish Association of Regional Anaesthesia and Pain Treatment. Pol Przegl Chir 91: 47-68.
- Elmowitz JS, Shupak RP (2009) Pharmacological and Non-Pharmacological Methods of Postoperative Pain Control Following Oral and Maxillofacial Surgery: A Scoping Review. J Oral Maxillofac Surg 79: 2000-9.
- Misiołek H (2018) Zajączkowska R, Daszkiewicz A, et al. Postoperative pain management - 2018 consensus statement of the Section of Regional Anaesthesia and Pain Therapy of the Polish Society of Anaesthesiology and Intensive Therapy, the Polish Society of Regional Anaesthesia and Pain Therapy, the Polish Association for the Study of Pain and the National Consultant in Anaesthesiology and Intensive Therapy. Anaesthesiol Intensive Ther 50: 173-99.
- Pasternak M, Woroń J (2020) Postextractional pain management. Ból 21: 1.
- Hah J, Mackey SC, Schmidt P (2018) Effect of Perioperative Gabapentin on Postoperative Pain Resolution and Opioid Cessation in a Mixed Surgical Cohort: A Randomized Clinical Trial. JAMA Surg 153: 303-11.
- Dirks J, Fredensborg BB, Christensen D, Fomsgaard JS, Flyger H, Dahl JB (2002) A randomized study of the effects of single-dose gabapentin versus placebo on postoperative pain and morphine consumption after mastectomy. Anesthesiology 97: 560-64.
- Dierking G, Duedahl TH, Rasmussen ML (2004) Effects of gabapentin on postoperative morphine consumption and pain after abdominal hysterectomy: a randomized, double-blind trial. Acta Anaesthesiol Scand 48: 322-7.
- Kinney MA, Mantilla CB, Carns PE (2012) Preoperative Gabapentin for Acute Post-thoracotomy Analgesia: A Randomized, Double-Blinded, Active Placebo-Controlled Study. Pain Pract 12: 175-83.
- Twycros R, Wilcock A, Charlesworth S, Mortimer J, Adamczyk A (2004) Palliative drugs.com therapeutic highlights: gabapentin. Polska Medycyna Paliatywna 3: 379-83.
- Holdcroft A, Berkley KJ (2006) Sex and gender differences in pain and its relief. In: McMahon SB, Koltzenburg M, editor. Wall and Melzack’s textbook of pain. Elsevier.

Tables at a glance
Figures at a glance