Non-Hodgkin’s Brain Lymphoma with Localized Metastasis to Soft Palate, A Case Report and Review of the Literature Pacific Northwest Kaiser, USA
Received Date: June 15, 2021 Accepted Date: July 15, 2021 Published Date: July 17, 2021
doi: 10.17303/jdoh.2021.8.105
Citation:Anahita Ghazi (2021) Non-Hodgkin’s Brain Lymphoma with Localized Metastasis to soft and hard palate, A Case Report and Review of the Literature Pacific Northwest Kaiser, USA. J Dent Oral Health 8: 1-9.
Abstract
Squamous cell carcinoma (SCC), being the most common type of oral malignancy, arises from the surface epithelium. Since changes appear on the surface of the oral cavity, cancer can be detected more easily by clinicians or even patients. Other oral malignancies such as lymphomas usually arise in the lamina propria, initially with intact surface epithelium, which can be harder to be detected. Here we are reporting an asymptomatic male patient who went to his dentist for yearly dental exam and cleaning. His dentist noticed a very subtle submucosal mass on the left side of the palate. No tooth related pathology or infection was noticed. Biopsy of the palatal mass showed B-Cell Lymphoma. Further work up, imaging and biopsies showed a brain mass, B-Cell lymphoma involving the left anterior skull base, extending to the pterygomaxillary fissure, pterygopalatine fossa and maxillary sinus. Clinical presentation of this lymphoma on soft palate as an asymptomatic submucosal mass and being the first presentation of the disease was rare.
Keywords:Brain Lymphoma; Lymphoma of Oral Cavity
Introduction
SCC accounts for more than 90% of oral malignancies which arises from surface epithelium. [1, 9,13] A variant of SCC known as verrucous carcinoma (VC) arises from surface epithelium as well, which shows a relatively better behavior. [6]Other oral malignancies being approximately 10% of all, arise in the lamina propria usually with intact surface, including lymphomas, malignant neoplasms of salivary gland tissue, different types of sarcomas, metastatic carcinomas and other rare malignancies. Early detection of oral cancer can save lives and is the goal of health care providers. Oral malignancies arising in the lamina propria can have an aggressive behavior and early detection of those is very crucial. Palatal submucosal masses can be benign or malignant salivary gland neoplasms. Benign salivary gland tumors are usually slow growing, encapsulated with no extension to the adjacent tissue or metastasis. Malignant salivary gland neoplasms can show variable behavior, some being low grade such as low grade mucoepidermoid carcinoma, or polymorphous low-grade adenocarcinoma, and some can be aggressive tumors.[2] Sarcomas arising from different types of tissue in the lamina propria, usually show aggressive behavior. Oral sarcomas are rare, reported as being 1% of oral malignancies.[7] Lymphomas occurring on the palate, can be primary lymphoma of the palate or extension of primary lymphoma from adjacent tissue to the palate, as localized metastasis.
Both of them are considered as extranodal lymphomas. [3,4,36] Here we report a case of extranodal brain lymphoma with localized metastasis to soft palate. The discussion has a review of literature regarding oral lymphomas.
Case Report
A seventy-three-year-old male patient went to Pacific Northwest Kaiser clinic for his yearly dental exam and cleaning. His medical history included history of colonic polyp, atherosclerosis of aorta, chronic rhinitis, sleep apnea, dyslipidemia, right carpal tunnel syndrome, knee joint pain and bilateral sensorineural hearing loss. He was on Lipitor for dyslipidemia. Patient had no mouth symptoms. His dentist noticed a subtle change on the left side of his palate [Figure 1] Upon palpation area was not tender and was slightly fluctuant. The surface mucosa was intact with no erythema or changes. No tooth related pathology or infection was detected.
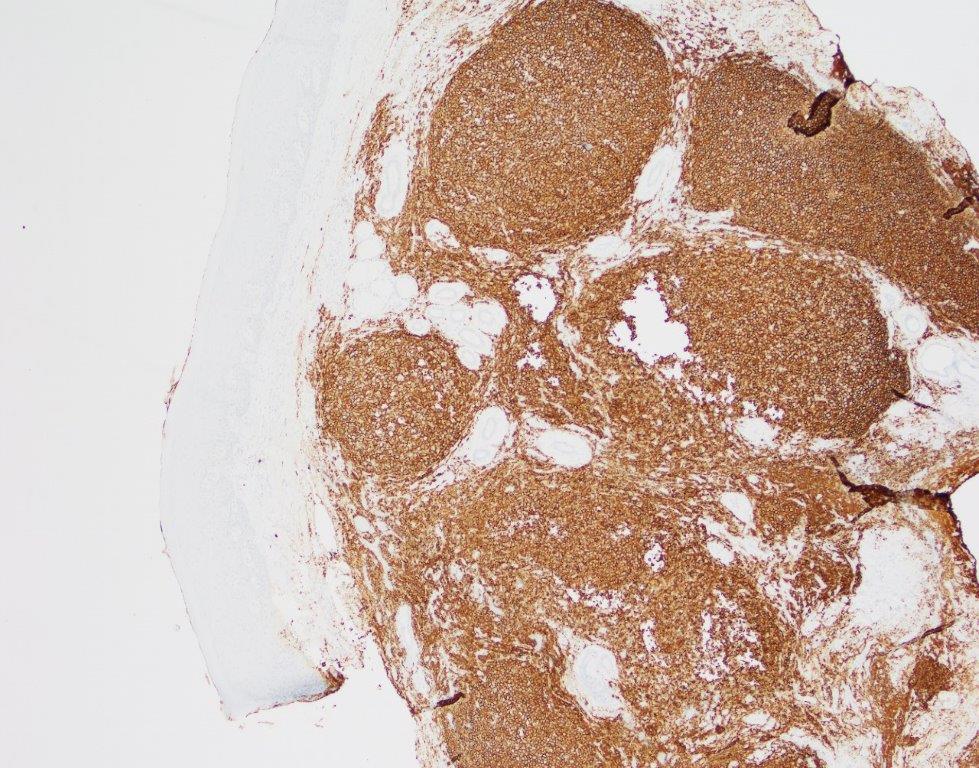
Patient was referred to oral pathology clinic at Pacific Northwest Kaiser. After clinical evaluation by oral pathologist, a palatal biopsy was recommended. Patient first declined the biopsy since he had no pain or symptoms. He could not feel the palatal asymmetry that he had, he stated. After reviewing the clinical photo with the patient and more explanation of the differential diagnosis, he agreed to get a biopsy done. An incisional biopsy was done and sent to Kaiser pathology lab. The result came out as “Atypical lymphocytic infiltrate” with a comment indicating the possibility of a B-Cell lymphoproliferative disorder. The pathologist recommended a second biopsy with additional fragments for flow cytometry. The second biopsy result was “CD20 positive B-Cell lymphoma with increased proliferation rate”. Figure 2, 3, and 4. With further imaging a brain mass was detected and subsequently a biopsy was done. Summary of findings and conclusion was Pterygomaxillary fissure / pterygopalatine fossa mass with extension/metastasis into the maxillary sinus and soft palate, B-Cell lymphoma. Patient went under the care of oncology.
Chemotherapy was recommended and done. Initial biopsy at oral pathology clinic was done in February 2019. Patient is done with his treatment course for more than a year now. He is doing well. Surveillance scan and follow up check and tests for his condition are still recommended. Presently all his test and imaging results are within normal limits.
Discussion
Lymphomas are a heterogeneous group of malignant diseases characterized by the proliferation of malignant lymphoid cells or their precursors. Lymphomas are the ninth most common cancer and constitute 3.2% of malignant tumors, which also account for 2.7% of cancer deaths worldwide.[8]
Traditionally, lymphomas are divided into two subtypes: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL), with differences in histology, clinical features, and prognosis.[9] NHL is further classified as B- or T-cell lymphomas. In B-lymphocyte group, two major categories are recognized: precursor and mature B-lymphocytes.[10] NHL and HL have been estimated to represent 4.3% and 0.5%, respectively, of all new cancer cases in the US in 2018.[11] It is non-Hodgkin’s lymphoma (NHL) which is having more extra nodal spread than Hodgkin’s lymphoma. Extranodal NHL sites can be gastrointestinal tract (GIT), CNS, skin, bone etc., out of which the oral cavity as a primary site of extra nodal lymphoma is even rarer.[12]
Up to 48% of NHLs occur in extranodal sites, with head and neck being the second most common frequent anatomic site of extranodal NHLs following the gastrointestinal tract. Half of the extranodal NHLs of the head and neck are located in the Waldeyer ring, which is an area encompassed by the nasopharynx, the tonsil and the base of the tongue. Extranodal lymphomas arising in the oral cavity account for less than 5% of all oral malignant neoplasms and are the most common nonepithelial malignant neoplasm in the oral cavity and maxillofacial region. They represent the third most frequent group of malignant lesions in the oral cavity, following squamous cell carcinoma and salivary gland neoplasms. [9,13]
Involvement of buccal mucosa, tongue, floor of the mouth and lips has been reported quite infrequently with approximately 2% of all extranodal lymphomas. When NHL appears extranodally in the oral cavity, it is usually indicative of widely disseminated disease. [15] Approximately 85% of these are located submucosally to the gingivae of the hard or soft palate and tongue.[9] The histologic types of NHLs that are especially common in the head and neck are the B-cell neoplasms: chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), extranodal marginal zone lymphoma of the mucosa-associated lymphoid tissue (MALT), nodal marginal zone lymphoma, follicular lymphoma (FL), diffuse large B-cell lymphoma (DLBCL), mantle cell lymphoma (MCL), and Burkitt lymphoma/leukemia (BL). Most of the extranodal NHLs of the oral cavity and maxillofacial region are of the DLBCL and MALT subtypes.[9] Both histopathological and immunohistochemical (IHC) analysis were strongly advisable for proper management and prognosis. [15]
Worldwide, DLBCL represents the most common sub-type (had extra space in between) of NHL, accounting for 30%–40% of all newly diagnosed cases. DLBCL typically presents as an aggressive lymphoma, evolving over months and resulting in symptomatic disease that would imminently be fatal without treatment.[19]
The clinical appearance of DLBCL is non-specific, most commonly presenting as a painless, swollen mass. The prevalence of DLBCL is increased in elderly patients, being on average most common in the 7th decade of life.[13] DLBCL is further classified as germinal center B-cell (GCB)-like and activated B-cell (ABC)-like and molecular subgroups, based on gene expression profiling (GEP) as well as a group of cases that could not be classified into either category. GCB and ABC subgroups differ in their chromosomal alterations, activation of signaling pathways and clinical outcome.[21] Non-immunosuppressed patients of any age can be affected, most patients being in the middle age group or older adult, with male preponderance. Patients with disseminated disease course and the presence of an immunosuppressed condition like AIDS have poor prognosis.[12] In HIV-infected individuals, patients with lymphoma are almost all men, who are overall younger individuals. [15] Epstein-Barr virus (EBV) and Human herpesvirus-8 (HHV8) have also been reported to accelerate the process in immunosuppressed patients causing Plasmablastic lymphoma (PBL) which is a subtype of DLBCL.[18] Currently, the R–CHOP regimen (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone) is the standard therapy for patients with DLBCL, which has a 60–70% cure rate.[20]
Unlike patients with nodal HL and NHL or extranodal HL and NHL in other organs, who more frequently present with B symptoms (fever greater than 38 °C; drenching night sweats; unintentional weight loss of at least 10% of their body weight over six months or fewer), patients with oral lymphoma (OL) seldom show B symptoms and mostly present with a swollen mass, followed by non-healing ulcerated lesions. [16,17,18,22] Other clinical presentations include hypermobile tooth, paresthesia, pain, palpable lymph nodes, facial asymmetry and inflammatory-like lesions. The oral manifestations of lymphomas are not specific, and are similar to many other diseases, such as advanced periodontal disease, pyogenic granuloma, peripheral giant cell granuloma, osteomyelitis or other malignancies encountered in the oral cavity.
Considering the radiographic findings of OL occurring in the jawbones, they are usually unspecific with the most frequent appearance is an osteolytic lesion with an ill-defined border. These findings are similar to those of other diseases with bony involvement, such as osteomyelitis, a deep fungal infection, or malignant lesions such as squamous cell carcinoma or salivary gland neoplasm. Review of Some previous studies revealed widening of the periodontal ligament space [23-29] and loss of the lamina dura [24,27-29] as some possible radiographic findings, which may mimic the presentation of advanced periodontal disease or tooth necrosis. Cases may also present with a periapical radiolucency resembling periapical lesions of endodontic origin on a periapical radiograph. [30-32] Clinical oral practitioners should be alert to these radiographic changes and correlate the clinical findings with the radiographic findings. If the radiographic features do not conform to the clinical findings, a biopsy is required for proper diagnosis since early detection and diagnosis could promote adequate treatment and a better prognosis. [11] Also, it is noteworthy to mention that lack of radiologic abnormalities does not exclude the possible presence of a small metastatic deposit in the oral bones.[36]
In most cases, the involvement of lymphomas in the oral cavity represents part of a disseminated disease; similar to this present case which seemed to happen secondary to primary B cell Lymphoma of the brain. Other metastatic tumors to the oral region are also uncommon and may occur either in the oral soft tissue or in the jawbones. Most common primary sources of metastatic tumors to the oral region in general are breast, lung, kidney, bone and colon.[36]
The majority of primary CNS lymphoma (PCNSL) in immunocompetent individuals are DLBCL. Indolent subtypes (usually small lymphocytic and lymphoplasmacytic lymphomas) are extremely rare. Immunodeficiency is the only established risk factor for the development of PCNSL; patients with HIV infection have a 3,600-fold increased risk compared with the general population. Our case, however, was not immunocompromised interestingly. In HIV-infected individuals, EBV infection is often detected; and in addition to DLBCL, classic or atypical brain lymphoma can be seen. In the immunocompetent patient, the median age at onset is in the 60th decade and EBV infection is usually absent. PCNSL is a rare subtype of NHL that is characterized by the primary and exclusive involvement of the brain, spinal cord, leptomeninges and eyes. It represents 4% of intracranial cancers and 4-6% of primary extranodal lymphomas. [33] Our attempt to analyze the information in the literature regarding metastatic tumors to the oral region posed several problems. Most of the information is presented in isolated case reports or in a very small series of cases. Moreover, in recent years, mainly unusual cases have been reported, which could cause some bias in favor of usual cases regarding the primary site and oral site.[36] However, it seems that brain lymphoma cases who manifested themselves solely as a local intraoral metastasic lesion have rarely been reported in the literature, thus making our case to be one of a very few of a kind.
Brain lymphoma may present with neurological symptoms based on the disease site: focal deficits, neuropsychiatric symptoms, seizures and manifestations of increased intracranial pressure.[33] Definitive diagnosis requires pathologic confirmation. The diagnostic procedure of choice is a stereotactic biopsy of the brain lesion, or, if ocular involvement is present, vitrectomy. CSF sampling demonstrating lymphoma cells on cytology or flow cytometry may also be sufficient. However, due to potential delay of diagnosis (and treatment) it is generally advisable to obtain a biopsy of an accessible brain lesion rather than obtaining CSF or vitreous fluid for assessment prior to biopsy. CSF and vitreous fluid can be used for cytological evaluation, immunophenotyping
and detection of immunoglobulin H or T-cell receptor rearrangements by PCR analysis indicating monoclonality. [35]
Regarding the treatment, unlike other primary brain tumors, PCNSL respond favorably to chemo- and radiation therapy. Unfortunately, survival is usually inferior in comparison to systemic, non-CNS lymphomas.[34]
In the present case, early detection of the palatal mass led to diagnosis and detection of the brain tumor. Patient was referred to medical for further work up and imaging. head/brain and brain MRI showed subdural hematoma, nodular soft tissue enhancement along the left cavernous sinus extending to the left foramen rotundum and large soft tissue mass in the region of the left pterygopalatine fossa. Biopsy results of the left palate oral mucosa showed an underlying nodular lymphoid infiltrate. The immuno-histochemical evaluation showed a prominent population of CD20 positive B-cells, which co-express CD10 and Pax-5 with weak bcl-6.
Flow cytometry demonstrates a monoclonal kappa light chain restricted B-cell population which expresses CD19, CD20, and CD 22 with possible partial CD10. No evidence of abnormal T-cell was found. All the findings were compatible with a CD10 positive B-cell lymphoma. EBV in situ staining was negative. The subsequent left pterygopalatine fossa mass biopsy also showed similar cellular composition of monoclonal B-cell population in less than 5% of total cells (low cellularity specimen) which was CD10 and CD20 positive with a scattered bcl-6 positivity and low-to-moderate proliferation rate with MIB-1. Lysed tissue specimen, neutrophils and dense fibrous tissue constituted the reminder of the specimen microscopically.
Hence, due to the rising incidence of extranodal lymphomas, it has become imperative not to take any swellings of the orofacial region at face value but to properly examine its pathology and treat it judiciously, especially where signs and symptoms persist in spite of treatment.
Conclusion
Occurrence of primary lymphoma in the pterygopalatine fossa with extension to maxillary sinus and soft and hard palate like this case, is rare. Thorough oral exams by clinicians, health care providers, dentists and hygienists are very crucial. Unfortunately, oral cancer, SCC or VC which appear on the surface epithelium, or other kinds which arise in the lamina propria can be painless at early stage. Unlike SCC and VC which show oral mucosal surface disturbances, other oral malignancies appear submucosally with intact surface. They can show surface changes like ulceration at later stage. As this case showed, early stage of oral cancer can be asymptomatic with subtle clinical features. This patient’s palatal lymphoma was caught early. Subsequently existence of the malignant neoplasm in adjacent areas was detected, which made the treatment course smooth and successful. Early detection of oral cancer can save lives.
- Migueláñez-Medrán BC, Pozo-Kreilinger JJ, Cebrián-Carretero JL, Martínez-García MA, López-Sánchez AF (2019) Oral squamous cell carcinoma of tongue: Histological risk assessment. A pilot study. Med Oral Patol Oral Cir Bucal 24: e603-9.
- Tian Z, Li L, Wang L, Hu Y, Li J (2010) Salivary gland neoplasms in oral and maxillofacial regions: a 23-year retrospective study of 6982 cases in an eastern Chinese population. Maxillofac Surg 39: 235-42.
- Jawanda Kaur Manveen, RV Subramanyam, Grewal Harshaminder, Shankari Madhu, Ravi Narula (2012) Primary B-cell MALT lymphoma of the palate: A case report and distinction from benign lymphoid hyperplasia (pseudolymphoma). J Oral Maxillofac Pathol 16: 97-102.
- Sujit Ranjan Sahoo, Satya Ranjan Misra, Lora Mishra, Sobhan Mishra (2014) Primary diffuse large B-cell lymphoma in the anterior hard palate: A rare case report with review of literature. J Oral Maxillofac Pathol 18: 102-6.
- Jawanda Kaur Manveen, RV Subramanyam, Grewal Harshaminder, Shankari Madhu, Ravi Narula. Primary B-cell MALT lymphoma of the palate: A case report and distinction from benign lymphoid hyperplasia (pseudolymphoma). Oral Maxillofac Pathol 16: 97-102.
- Alkan A (2010) Oral verrucous carcinoma: a study of 12 cases. Eur J Dent. 2010.
- Tomoki Sumida, Naruto Otawa, Y U Kamata, Tomohiro Yamada, Kenichiro Uchida, et al. (2015) A Clinical Investigation of Oral Sarcomas at Multi-institutions Over the Past 30 Years. Anticancer Res 35: 4551-5.
- J. Ferlay, I. Soerjomataram, R. Dikshit, S. Eser, C. Mathers, M. Rebelo, et al. (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Canc 136: E359-E386.
- Triantafillidou K (2012) Extranodal Non-Hodgkin Lymphomas of the Oral Cavity and Maxillofacial Region: A Clinical Study of 58 Cases and Review of the Literature. J Oral Maxillofac Surg.
- Narang RS, Manchanda AS, Kaur H (2019) Evaluation of a case of diffuse large B-cell lymphoma. J Oral Maxillofac Pathol 23: 7-11.
- Tseng CH, Wang WC, Chen CY, Hsu HJ, Chen YK (2021) Clinical manifestations of oral lymphomas - Retrospective study of 15 cases in a Taiwanese population and a review of 592 cases from the literature. J Formos Med Assoc 120: 361-70.
- Batta N, Shukla M, Pandey M (2019) Natural course of diffuse large B cell lymphoma—a manifestation in buccal mucosa. World J Surg Oncol 17: 219.
- A. Kolokotronis, N. Konstantinou, I. Christakis, P. Papadimitriou, A. Matiakis, et al. (2005) Localized B-cell non-Hodgkin's lymphoma of oral cavity and maxillofacial region: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99: 303-10.
- Maheshwari Gopal Krishna, Baboo Harshad Acharatlal, Shah Nilesh Manubhai. Primary non-Hodgkin’s lymphoma of the oral tongue. Turkish Journal of Cancer 31: 121–4.
- Reddy I, GS Reddy, YR Prakash AR, TRS (2014) Non-Hodgkin’s Lymphoma in Buccal Vestibule -Case Report. J Clin Diagn Res 8: QD01-2.
- Kemp S (2008) Oral non-Hodgkin’s lymphoma: review of the literature and World Health Organization classification with reference to 40 cases. Oral surg Oral med Oral Pathol Oral Radiol Endod 105: 194–201.
- Epstein JB, Epstein JD, Le NDGorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92: 519–25.
- Corti M (2015) Primary extranodal non-Hodgkin lymphoma of the head and neck in patients with acquired immunodeficiency syndrome: a clinicopathologic study of 24 patients in a single hospital of infectious diseases in Argentina. Int Arch Otorhinolaryngol 19: 354–8.
- Sehn LH, Gascoyne RD (2015) Diffuse large B-cell lymphoma: Optimizing outcome in the context of clinical and biologic heterogeneity. Blood 125: 22–32.
- S Li, KH Young, LJ Medeiros (2018) Diffuse large B-cell lymphoma Pathology 50: 74-87.
- Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. (2016) The 2016 revision of the world health organization classification of lymphoid neoplasms. Blood 127: 2375–90.
- JO Guevara-Canales, R Morales-Vadillo SJ, Sacsaquispe-Contreras C (2013) Barrionuevo-Cornejo, J. Montes- Gil, C.E. Cava-Vergiu, et al. Malignant lymphoma of the oral cavity and the maxillofacial region: overall survival prognostic factors. Med Oral Patol Oral Cir Bucal 18: e619-e626.
- CM Spatafore, G Keyes, AE Skidmore (1989) Lymphoma: an unusual oral presentation. J Endod 15: 438-41.
- W Nittayananta, S Apinawatavorngul, S. Chungpanich, S. Pongpanich, S. Kietthubthe. Burkitt-like lymphoma presenting as a periodontal disease in AIDS patients: a report of two cases. Oral Dis 4: 281-4.
- AC Chi, RL Coles, CL Ledford, BW Neville, J Lazarchick (2012) Spindle cell lymphoma of the oral cavity: a case report and review of the literature. J Oral Maxillofac Surg 70: 2229-37.
- Y Mochizuki, H Harada, K Sakamoto, K Kayamori, S Nakamura, et al. (2015) Malignant lymphoma with initial symptoms in the mandibular region. J Canc Ther 6: 554-65.
- RNF Silva, EF Mendonca, AC Batista, RCG Alencar, RA Mesquita, NL (2019) Costa.T-cell/histiocyte-rich large B-cell lymphoma: report of the first case in the mandible. Head Neck Pathol, 13: 711-7.
- L Eisenbud, J Sciubba, R Mir, SA Sachs (1983) Oral presentations in non-Hodgkin's lymphoma: a review of thirty-one cases. Part I. Data analysis. Oral Surg Oral Med Oral Pathol 56: 151-6.
- BH Cho, DH Shin, YH Jung, HR Park (2018) Widely disseminated sporadic Burkitt lymphoma initially presented as oral manifestations in a 6-year-old boy. J Oral Biol Craniofac Res 8: 140-2.
- DL Pereira, DT Fernandes, AR Santos-Silva, PA Vargas, OP de Almeida, et al. (2015) Intraosseous non-Hodgkin lymphoma mimicking a periapical lesion. J Endod 41: 1738-42.
- D MacDonald, T Li, SF Leung, J Curtin A Yeung, MA Martin (2017) Extranodal lymphoma arising within the maxillary alveolus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol 17: e233-e238.
- MS Kumar, A Gannepalli, A Chandragiri, K Amarnath (2016) Diffuse large B-cell lymphoma of maxilla – a case report of late relapse. J Clin Diagn Res 10.
- Barbara Vannata, Emanuele Zucca. Primary extranodal B-cell lymphoma: current concepts and treatment strategies. Chinese Clinical Oncology Mar;4: 10.
- Grommes C, Rubenstein JL, DeAngelis LM, Ferreri AJM, Batchelor TT (2019) Comprehensive approach to diagnosis and treatment of newly diagnosed primary CNS lymphoma. Neuro Oncol 21: 296-305.
- Scott BJ, Douglas VC, Tihan T, Rubenstein JL, Josephson SA (2013) A systematic approach to the diagnosis of suspected central nervous system lymphoma. JAMA Neurol 70: 311–19.
- A Hirshberg and A Buchner (1995) Metastatic Tumours to the Oral Region. An Overview. Eur J Cancer B Oral Oncol 31: 355-60.

Figures at a glance