Stigmatisation of People Living with HIV/AIDS in Burkina Faso: Multilevel Socioecological Analysis of Determinants
Received Date: April 19, 2021 Accepted Date: May 19, 2021 Published Date: May 22, 2021
doi: 10.17303/jaid.2021.8.104
Citation: Mikaila Kabore (2021) Stigmatisation of People Living with HIV/AIDS in Burkina Faso: Multilevel Socioecological Analysis of Determinants. J HIV AIDS Infect Dis 8: 1-12.
Abstract
Background: Stigmatisation of people living with HIV/AIDS (PLHIV) negatively influences the response to the disease. Our goal was to identify the individual and contextual determinants of population's stigma towards PLHIV in Burkina Faso.
Methods: Secondary data set from the fourth DHS conducted in 2010 were analyzed. The study included those who answered "yes" to the question «if they had ever heard about HIV/AIDS». Thus, the final sample included 16,571 women and 7,102 men. We performed a multilevel logistic regression with MLwiN software. The contextual level was the thirteen regions of the country.
Results: 23,673 individuals (15–59 years) were surveyed, of which more than one-third (36.8%) were under 25 years old. The prevalence of stigma was 89% [95% CI: 88.59%−89.45%] (women: 92.70% versus men: 87.10%, p<0.001). At the individual level, sociocultural factors (lack of knowledge about HIV/AIDS OR=2.41***, inaccessibility to media OR=1.60***, not doing the HIV test OR=1.34***) and sociodemographic factors (young age OR=1.39***, female sex OR=2.08***, rural area OR=1.29***) seemed to be more associated with stigmatising behaviours than economic factors. At the contextual level, access to media (OR=1.70***) and knowledge about HIV contextual (0.70***) influenced stigmatising behaviour of individuals towards PLHIV.
Conclusions: Young people, female, less educated, with low knowledge about HIV/AIDS, living in the countryside with a low socioeconomic level were more likely to stigmatise PLHIV. Therefore, there is a need to strengthen awareness programs through mass media for the benefit of this population, with the aim to move towards UNAIDS "zero discrimination" goal.
Keys words: Burkina Faso; Determinants; People living with HIV/AIDS; Socioecological; Stigma
Introduction
Voluntary HIV testing followed by the care of infected persons is recognised as one of the main ways of reducing the transmission of the disease [1]. However, according to the Demographic and Health Surveys (DHS) conducted in various countries south of the Sahara, few people had been tested for HIV and received their results in the last 12 months [2,4]. This is partly due to rejection, contempt, devaluation and exclusion of people living with HIV (PLHIV) from society because of their status. This situation hampers the momentum towards knowledge of HIV status, thus early treatment [5].
For a long time, experts and communities have consistently identified the stigma and discrimination of PLHIV as key factors in the spread of infection and major obstacles to effective HIV control in all regions of the world [5,7]. According to Smart [8], HIV/AIDS-related stigma is a real or perceived negative response from individuals, the community, or society to one or more people.
In Burkina Faso, according to the 2010 DHS, 82% of men and 92% of women had stigmatising attitudes towards PLHIV [4]. Victims of stigma and discrimination mention several negative effects, including loss of income, and isolation in the community, the lack of active social participation due to HIV status, feelings of guilt, shame and suicidal thoughts [9].
Many studies have described the factors associated with negative attitudes that individuals develop towards PLHIV. Factors frequently taken into account are sociodemographic [10,13], the level of knowledge about HIV prevention and transmission modes [10,14,16], the experience of contact with an infected person by HIV [17] or with a voluntary counselling council's’ structure[11,18]. However, little research has incorporated the influence of the social environment on these individual attitudes towards PLHIV. Those who examined it [19] did not consider the prevalence of HIV in the community and the influence of the media in their analyses, whereas these factors can shape the perception that individuals have of the disease and hence their behaviour towards PLHIV.
Based on these findings, we proposed to integrate the level of knowledge of HIV/AIDS and its prevalence in the community, as well as the influence of the media to analyse individual and contextual determinants that could be at the origin of negative attitudes of the population of Burkina Faso to people living with HIV/AIDS. In other words, how can socio-demographic, cultural and economic factors, community factors including HIV-related knowledge, HIV prevalence and the media influence the attitude of individuals towards PLWHIV in Burkina Faso?
Methods
Study framework
This study covered all thirteen regions of Burkina Faso whose differences in knowledge of the disease, media availability and HIV prevalence may influence individuals' behaviours with people living with HIV.
Study Population and Data
Study population
It consisted of all women (15–49 years) and men (15–59 years) interviewed in the context of the fourth Demographic and Health Survey and Multiple Indicators of Burkina Faso conducted in 2010 (EDSBF-MICS -IV).
Data
We used the database of the EDSBF-MICS-IV. This survey was initiated by the government and executed by the National Institute of Statistics and Demography (INSD) in collaboration with ICF International's World Demographic and Health Surveys Program (DHS MEASURE). Conducted from May 2010 to early January 2011, its objective was to estimate many socio-economic, demographic and health indicators at the level of the entire population. One of the specific objectives was to assess the level of knowledge, opinions and attitudes towards sexually transmitted infections (STIs) and HIV/AIDS among respondents [4].
Sampling
It was a stratified national sample drawn at two levels from 14 947 households. Of these, 14 536 were employed at the time of the survey and 14 424 were successfully interviewed (99%). Within 14 424 households, 17 363 women were identified as eligible, of whom 17 087 were interviewed (98%). Eligible were women who usually live-in households selected or present the night before the survey. Men, meanwhile, were interviewed in one of two households or 7 506 identified and 7 307 successfully surveyed (97%) [4]. The study was limited to those who answered "yes" to the question of whether they had ever heard of HIV/AIDS, giving a final sample of 16 571 women and 7 102 men.
Study variables
Outcome variable
Four questions evoked stigmatising behaviours that respondents could have for PLHIV. It was: (1) "Would you be ready to take care of the home of a parent with the AIDS virus? (2) "Would you buy fresh vegetables from a trader living with the AIDS virus? (3) "Do you think that a teacher living with the AIDS virus who is not sick should be allowed to continue teaching? (4) "Do you think that it is not necessary to keep the status of a family member with the AIDS virus secret? “
As part of our study, we created a dependent variable called "PLHIV Stigma" that aggregated the sum of responses to these four questions. Thus, the two modalities of the dependent variable were:
"No = 0", if the respondent does not adopt stigmatizing attitudes otherwise, if none of the answers to the four questions posed were negative for PLHIV.
"Yes = 1", if at least one of the responses given was negative for PLHIV
Independent variables
They were grouped at two levels, namely individual (sociodemographic, cultural and economic variables of the respondents) and contextual:
At the Individual Level
• Sociodemographic variables included age, sex, marital status, and place of residence.
• Age has been transformed into three classes: 15 to 24, 25 to 34, 35 and over.
• Marital status was grouped into two categories: living as a couple (married, living with a partner), and living alone (never in a union, single, separated, and divorced).
• Cultural variables included religion, media accessibility, testing, and level of knowledge about HIV/AIDS.
• Media accessibility included questions including: how often to read a newspaper? how often to listen to the radio? and how often you watch television?
• The voluntary screening test raised the question: “Have you ever tested whether you have the AIDS virus?”
• The level of knowledge on HIV/AIDS included prevention and modes of transmission. Ten (10) questions were the basis for assessing the level of knowledge of populations about the disease. A variable “level of knowledge about HIV” that is the sum of the first nine variables (the last one with a nonresponse rate of 11.0% was discarded) referring to the means of prevention and modes of HIV transmission was created. A summative index is obtained from the nine responses and then grouped into the variable into three categories namely level of knowledge “zero” for individuals who correctly answered most two questions; “low” level for those who answered correctly between three and six of nine questions and “high” for those who answered at least seven of the nine questions correctly.
• The economic variables included the economic standard of living, the level of education and professional activity.
• The factorial scores of the proxy Wealth Index Factor approximated the economic standard of living. The variable was grouped into two categories: “poor” and “not poor”.
• Professional activity includes unemployed, working in the informal sector (unskilled manual labour) and working in formal sector (administrative activities).
At the contextual level
• -The area of residence at the time of the survey was our aggregation variable. The choice of this variable is justified by the fact that each region presents, in terms of geographical, socio-economic, cultural and health, specificity likely to influence the behaviour of individuals with regard to HIV/AIDS. Three variables were used to measure the contextual effect. It was:
• The contextual level of access to media: this variable measures the proportion of respondents who are often exposed to the media by region. It coded in two modalities: low level for contexts whose proportion is lower than the average of the regions and high level otherwise.
• The contextual level of knowledge on HIV: it represents the proportion of respondents with a good knowledge of the disease in each region. It was coded in two modalities: low level for contexts whose proportion is lower than the average of the regions and high level otherwise.
• The contextual HIV prevalence: it represents the prevalence of HIV in each region. It was coded in two ways: weak for contexts with prevalence lower than the national level and high if not.
Analytical methods
The analysis of the survey data consisted of:
A descriptive step that made it possible to assess the distribution of the variables under study;
A bivariate analysis that made it possible to look for the link between each independent variable and the variable to be explained (the stigmatisation of PLHIV);
Finally, an explanatory analysis using the multilevel regression model with the MLwiN 2.30 software, to identify the effect of individual and contextual factors in the stigmatisation of PLHIV.
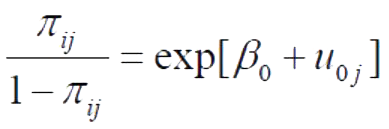
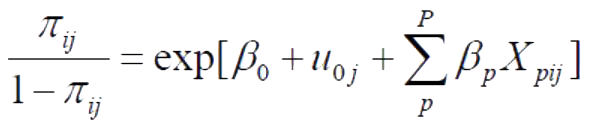
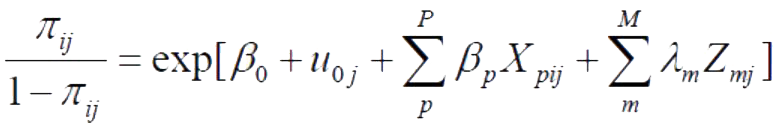
The analyses led to the construction of five models of analysis.
First, it was the "empty model" or variance analysis model with no explanatory variables. The goal is to decompose the initial variance to appreciate the part attributable to the different levels of analysis. The values provided by the "empty model" (model 1) were used as a reference for the future and enabled the impact of the explanatory variables introduced in the subsequent models to be evaluated.
Then, we successively introduced from model 2 to model 5, the individual and then contextual variables by the group of factors, to judge the evolution of the contextual variance. During these analyses, the significance level p was 5% and was materialised by stars (*)
As follows: ˂ 1% (***), ˂ 5% (**) and ˂ 10% (*). Table 1 summarises the five models of analysis in our study.
Results
The extent of stigmatisation of PLHIV
The prevalence of PLHIV stigma in Burkina Faso was 89.0% with a 95% confidence interval [88.59% - 89.45%]. The regions with the highest prevalence were Boucle du Mouhoun, North Central and Sahel with 95.20%, 94.10% and 93.90% respectively. Central Plateau, Central and Eastern Region had the lowest prevalence with 85.40%, 81.30% and 79.20%, respectively (Figure 1).
Bivariate analysis of the factors associated with the stigmatisation of PLWHA
Age (p <0.001), sex (p <0.001), marital status (p <0.001) and place of residence (p <0.001) were the sociodemographic determinants of PLHIV stigma. At the cultural level, religion (p <0.001), media exposure (p <0.001), having previously tested for HIV (p <0.001) and level of knowledge about HIV/AIDS (p <0.001) were the determining factors found. Finally, work status (p <0.001), Household wealth (p <0.001) and education’s level (p <0.001) were the economic determinants that could explain the stigmatisation of PLHIVs (Table 2).
The explanatory analysis of the determinants of the stigmatisation of PLHIV
This analysis made it possible to see the effect of individual and contextual factors on the stigmatising behaviour of populations towards PLHIV.
The empty model presents the average phenomenon β0 = 7.622. An analysis of its variance shows that the stigmatisation of PLHIV varied by region. Indeed, = 0.748 was statistically significant.
After introducing the socio-demographic factors into the model, we found that age, sex, and place of residence significantly influenced the stigmatising behaviours of individuals towards PLHIV. The contextual variance remained highly significant ( = 0.778).
Taking sociocultural factors into account as a result of socio-demographic factors in this model decreased the effect of sociodemographic variables, especially the age, sex and place of residence of the respondents, but not significantly, except for 35 years and older who no longer influenced the stigmatisation of PLHIV. In addition, it appears that religion, ability to perform HIV testing, access to media and knowledge about HIV were associated with stigma.
The economic factors taken into account in the model contributed to explaining stigmatising behaviours towards PLHIV without influencing the effect of other factors, particularly sociodemographic and cultural factors. Outside the standard of economic life, education and occupation significantly influenced the stigmatising behaviours of individuals.
The entry of contextual factors in the final model reduces the contextual variance by 3.08% compared to the empty model but not significantly. In addition, there is no significant variation in the effect of the individual characteristics of those surveyed on the stigmatisation of PLHIV after considering contextual factors. Ultimately, all sociodemographic, socio-cultural and economic factors (except standard of living of households) and contextual factors, notably the level of knowledge about HIV and access to the media, are determinants of the stigmatisation of PLHIV.
Age range is a key determinant of stigmatisation. Indeed, young people (15-24 years) are 1.40 times more likely to have stigmatising behaviour than others are (over 25 years). Regarding sex, women are stigmatised at 2.09 times than men. Individuals living alone were more likely to be stigmatised than those living in couples (1.13 times). Religion is also a determinant of stigmatisation of PLHIV. Muslims and those of other religions (animist and non-religious) were, respectively 1.26 times and 1.23 times more likely, than Christians to have stigmatising attitudes. In the case of media access, inaccessibility increased the risk of stigmatisation by 1.59. In terms of performing the screening test, individuals who had never tested were at a higher risk of stigmatisation (1.33 times) than those who have tested. In terms of knowledge about prevention and modes of HIV transmission, the lack of knowledge increases the risk of stigmatisation by 2.39 times higher than the level of knowledge, and the low level of knowledge increased the risk at 1.39 times. As for education, the uneducated were 2.50 times more likely than those with secondary and higher education. Regarding occupation, respondents in the informal sector were 1.12 times more likely than their counterpart in the formal sector.
At the contextual level, in regions with high media accessibility, the risk of stigmatisation increased by 1.20 compared to other regions. In high HIV knowledge-level settings, the risk of stigmatising PLHIV decreased by 0.70 regardless of the individual level of knowledge about HIV/AIDS. The contextual seroprevalence of HIV did not significantly influence stigmatising behaviours.
In terms of the contribution of factors to the explanation of the stigmatisation of PLHIV, cultural factors appeared to be the most important, before socio-demographic and economic factors. Table 3 summarizes the results of the analysis of individual and contextual determinants of PLHIV stigma.
Discussion
This study analysed the individual and contextual determinants of the negative attitudes of populations towards PLHIV. Given its importance and impact on HIV prevention efforts in Burkina Faso, the stigma and discrimination of PLHIV is a real obstacle in the response to the disease. The discussion of our results focused on four points according to the groups of determinants taken into account in the analysis.
Sociodemographic factors
This study noted that age, sex, marital status, and place of residence were factors that contributed to stigmatising behaviours towards PLHIV. It revealed that these negative attitudes were more prevalent among young people (15-24 years) than adults, so women were more likely than men, as well as non-couples and those living in rural areas. Other studies made the same observations. Indeed, Chiao [19] in Kenya and Letamo [15] in Botswana found that individuals younger than 25 years had less tolerance attitudes towards PLHIV than adults. The first study involved people living in couples who were less tolerant of AIDS patients. The influence was not significantly significant in Botswana on marital status. The stigma attached to HIV/AIDS and the resulting discriminatory attitudes creates an environment promoting the spread of the virus. Strengthening HIV/AIDS education programmes, especially for young people and female sex can play an important role in reducing the stigma and discrimination of PLHIV.
Cultural factors
In some systems of traditional and religious beliefs everywhere, on health and illness, ancestors and God are the ultimate cause of the disease. With the advent of HIV/AIDS, these beliefs have been reinforced in many African countries, resulting in stigmatising behaviours towards PLHIVs. In our study, Muslims and individuals practising other religions (traditional and without religion) are recognized to have further stigmatising attitudes than Christians (Catholics and Protestants). These results corroborate those found by Chiao in Kenya [19], but were not significant.
The written and audio-visual media in general are the most widespread and accessible means of communication for the majority of the population. They can change the behaviour of individuals towards PLWHAs according to the information conveyed. Individuals who never had access to the media and those who had never been tested for HIV were more likely to have stigmatising attitudes. Several authors including Chiao [19] in Kenya, Babalola [20] and Fakolade [21] all in Nigeria, Chen [10] in China have achieved the same results on the positive influence of the mass media in the reduction of stigma related to HIV/AIDS. Thus, thanks to the awareness and information conveyed about the disease, people improve their knowledge about the means of prevention, transmission’s modes and the manifestation of the disease’s symptoms. This opportunity may lead to the end of the fear of infection caused by ignorance, misinformation, and lead to better acceptance of people with AIDS [22,23]. This study shows that individuals with no or low knowledge about HIV were more likely to scorn PLHIV. This finding is consistent with previous Letamo [15], Lau & Tsui [12], Chen [10]; Chiao [19], Shisana [16], all of whom confirmed that the low level of knowledge about HIV/AIDS is associated with stigmatising behaviours place of PLWA. Public health programs reducing HIV-related stigma need to focus more on communication media (media) and teaching curricula to strengthen information, awareness and education about HIV/AIDS the place of the general population and young layers in particular.
Economic factors
Education conditions the professional activity of individuals, their standard of living and their accessibility to information, particularly on HIV/AIDS. During the study, the absence or low level of education and the area of informal activity were identified as being associated with stigmatising behaviours towards PLHIVs. Similar results have been found by other authors, particularly in Botswana [15], Kenya [19] and China [10]. Informal activities are of a traditional nature and are conducted by unqualified people with a low level of education, which can be correlated with a low level of knowledge about HIV, which could explain their stigmatising attitudes towards PLHIVs. The standard of living was not significant in adopting stigmatising behaviours when reading our results.
Contextual factors
Regardless of individual characteristics, individuals living in high-level HIV/AIDS knowledge contexts tended to stigmatise PLHIVs less. However, the strong media influence tended to lead individuals living in these environments to more stigmatising behaviours. This negative community influence of the media on stigma could be explained by the fact the content of the messages that are disaggregated and their degree of concordance with the cultural values of the target audiences. The results were inconclusive for the seroprevalence of the disease. In sum, the idea that HIV-related stigma is less a question of individual characteristics than a social process built through cultural influences would be verified [10,19].
Limits were identified during the study that would be important to consider:
• Since the database is already established, some variables are missing from the analysis, particularly those assessing the knowledge of the respondents on the symptoms and treatment of HIV/AIDS, which would allow a more global assessment of the level of knowledge of individuals on HIV/AIDS infection.
• The survey was performed in the population, in addition the lack of qualitative data collected from this population and PLHIV did not allow to apprehend the level of stigmatisation felt by the latter themselves, nor the root causes of these negative behaviours of individuals and their impact on the lives of PLHIVs.
• The database is ten years old (2010). However, this is the last DHS survey conducted in the country and it corresponds to a period when HIV was still relatively more prevalent in the country and in the minds of the population. This again becomes an opportunity to address this issue of HIV-related stigma.
Conclusion
Our study found a very high prevalence of stigmatisation of individuals against PLHIV in Burkina Faso. The determining factors were present at both the individual and the contextual level. In fact, it appears that the negative behaviours towards PLHIVs came more from young, female, rural, Muslim or animist individuals without access to the media, as they did not never voluntarily do their HIV test, with a low level of education and knowledge of HIV, and finally evolving in an informal sector of activity. The behaviours of these individuals are also influenced by the environment in which they reside, including the degree to which media are located in their area and the information conveyed, as well as the level of knowledge of HIV/AIDS in their residential community, regardless of their background. Individual characteristics. All of this involves nationwide actions for these specific groups to reduce the stigmatisation of people with AIDS.
Acknowledgements
The authors are grateful to the Institute Superior des Sciences de la population (ISSP) in Burkina Faso and their teachers, especially Dr Nathalie Sawadogo. In addition, they are grateful to Professor Nicolas Meda for his guidance and expertise during this work.
Competing interest
The authors declare that they have no competing interest.
- Kilewo C, Massawe A, Lyamuya E, Semali I, Kalokola F, et al. (2001) HIV Counseling and Testing of Pregnant Women in Sub-Saharan Africa: Experiences From a Study on Prevention of Mother-to-Child HIV-1 Transmission in Dar Es Salaam, Tanzania. J Acquir Immune Defic Syndr 28: 458‑62.
- Institut national de la statistique (2016) Enquête par grappes à indicateurs multiples au Mali (MICS-Mali), 2015, Rapport final. Bamako, Mali: INSTAT.
- Institut National de la Statistique (INS) (2013) Enquête Démographique et de Santé et à Indicateurs Multiples du Niger 2012. Calverton, Maryland, USA : INS et ICF International.
- INSD, ICF International (2012) Enquête Démographique et de Santé et à Indicateurs Multiples (EDSBF-MICSIV) 2010. Burkina Faso. Calverton, Maryland, USA.
- UNAIDS (2020) UNAIDS data 2020. 2nd edition. Geneva, Switzerland: UNAIDS.
- Nyblade LC (2006) Measuring HIV stigma: Existing knowledge and gaps. Psychol Health Med 11: 335‑45.
- Parker R, Aggleton P (2003) HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 57: 13‑24.
- Smart R (2007) Module 1.4: Stigmatisation et discrimination liées au VIH et au sida. UNESCO-IIEP–EduSector AIDS Response Trust (ESART).
- ONUSIDA (2013) Rapport mondial : Rapport ONUSIDA sur l’épidémie mondiale de sida 2013. Genève : ONUSIDA.
- Chen J, Choe MK, Chen S, Zhang S (2007) The effects of individual- and community-level knowledge, beliefs, and fear on stigmatization of people living with HIV/AIDS in China. AIDS Care 19: 666‑73.
- Corno L, de Walque D (2013) Socioeconomic determinants of stigmatization and HIV testing in Lesotho. AIDS Care 25(sup1): S108‑13.
- Lau JTF, Tsui HY (2002) Surveillance of HIV/AIDS-Related Attitudes and Perceptions among the General Public in Hong Kong from 1994 to 2000. AIDS Educ Prev 14: 419‑31.
- Macintyre K, Brown L, Sosler S (2001) “It’s Not What You Know, But Who You Knew”: Examining the Relationship Between Behavior Change and AIDS Mortality in Africa. AIDS Educ Prev 13: 160‑74.
- Chen J, Choe MK, Chen S, Zhang S (2005) Community Environment and HIV/AIDS-Related Stigma in China. AIDS Educ Prev 17: 1‑11.
- Letamo G (2003) Prevalence of, and factors associated with, HIV/AIDS-related stigma and discriminatory attitudes in Botswana. J Health Popul Nutr 21: 347‑57.
- Shisana O, Human Sciences Research Council, Centre for AIDS Development, Research and Evaluation, South African Medical Research Council, National Institute for Communicable Diseases (South Africa) (2009) South African national HIV prevalence, incidence, behaviour and communication survey, 2008: A turning tide among teenagers. Cape Town: HSRC Press.
- Lau JTF, Tsui H (2006) Comparing the magnitude of discriminatory attitudes toward people living with HIV/AIDS and toward people with mental illness in the Hong Kong general population. Health Educ Res 22: 139‑52.
- Kalichman SC (2009) HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect 79: 442‑7.
- Chiao C, Mishra V, Sambisa W (2009) Individual- and community-level determinants of social acceptance of people living with HIV in Kenya: Results from a national population-based survey. Health Place 15: 742‑50.
- Babalola S, Fatusi A, Anyanti J (2009) Media saturation, communication exposure and HIV stigma in Nigeria. Soc Sci Med 68: 1513‑20.
- Fakolade R, Adebayo SB, Anyanti J, Ankomah A (2010) The impact of exposure to mass media campaigns and social support on levels and trends of HIV-related stigma and discrimination in Nigeria: Tools for enhancing effective HIV prevention programmes. J Biosoc Sci 42: 395‑407.
- Boer H, Emons PAA (2004) Accurate and inaccurate HIV transmission beliefs, stigmatizing and HIV protection motivation in northern Thailand. AIDS Care 16: 167‑76.
- Brown L, Macintyre K, Trujillo L (2003) Interventions to Reduce HIV/AIDS Stigma: What Have We Learned? AIDS Educ Prev 15: 49‑69.

Figures at a glance