First Case Report of Erythema Elevatum Diutinum Involving the Glans Penis of A HIV–Positive Patient: Possible Atypical Manifestation of Immune Reconstitution Inflammatory Syndrome
Received Date: July 29, 2020 Accepted Date: August 08, 2020 Published Date: August 11, 2020
doi: 10.17303/jaid.2020.7.103
Citation:: E. Petrie (2020) First Case Report of Erythema Elevatum Diutinum Involving the Glans Penis of A HIV–Positive Patient: Possible Atypical Manifestation of Immune Reconstitution Inflammatory Syndrome. J HIV AIDS Infect Dis 7: 1-7.
Abstract
We present a Human Immunodeficiency Virus (HIV)-positive patient who developed localized leukocytoclastic vasculitis (LCV) with histologic features of erythema elevatum diutinum on the glans penis after a change of antiretroviral treatment, suggestive of a form of immune reconstitution inflammatory syndrome (IRIS). Since the penile lesion in this patient occurred following a change of his antiretroviral regimen and persisted after several courses of antibiotics, we hypothesize that this phenomenon represents an atypical manifestation of IRIS. EED involving the penis is a very rare occurrence and could pose significant diagnostic challenges, particularly in HIV patients.
Keywords: HIV/AIDS; leukocytoclastic vasculitis; immune reconstitution inflammatory syndrome; skin lesion
Introduction
Leukocytoclastic vasculitis (LCV), a form of cutaneous small-vessel vasculitis, is characterized histologically by fibrinoid degeneration of the vessel wall of small capillaries in the dermis associated with neutrophilic infiltrate, perivascular nuclear dusts, and extravasation of red blood cells. Erythema elevatum diutinum (EDD), a chronic fibrosing form of leukocytoclastic vasculitis, has been reported in HIV-positive patients [1-3]. In a recent review of the literature on EED, Doktor et al [1] have identified a total of 133 cases of EED with 21 cases associated with HIV for an incidence of 16%. In fact, EED has emerged as a new specific Human Immunodeficiency Virus (HIV) associated with dermatosis. The investigators hypothesized immune complex deposition in the small vessels, triggered by either HIV or another infectious agent, as a possible mechanism for EED in HIV patients. The current report documents an unusual case of the localized fibrosing form of leukocytoclastic vasculitis on the penis of an HIV patient, which most likely represents an atypical manifestation of EED or the so-called "localized chronic fibrosing vasculitis" [2]. Since the penile lesion occurred after a change of the patient's antiretroviral treatment, we postulate that the lesion might represent a noninfectious manifestation of immune reconstitution inflammatory syndrome (IRIS).
Case summary
A 70-year old white man who had been positive for HIV for 21 years with a CD4 count of 577 cells/mL and an HIV viral load less than 20 copies/mL, presented in April 2016 for his HIV management. He previously received tenofovir disoproxil fumarate/emtricitabine (Truvada), ritonavir (Norvir), and fosamprenavir (Lexiva) as therapy for his immunocompromised condition. His past medical history included syphilis, diabetes, open-heart surgery, and partial colectomy due to colon cancer. The patient's colon cancer was in remission. His treatment was changed to elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide (Genvoya).
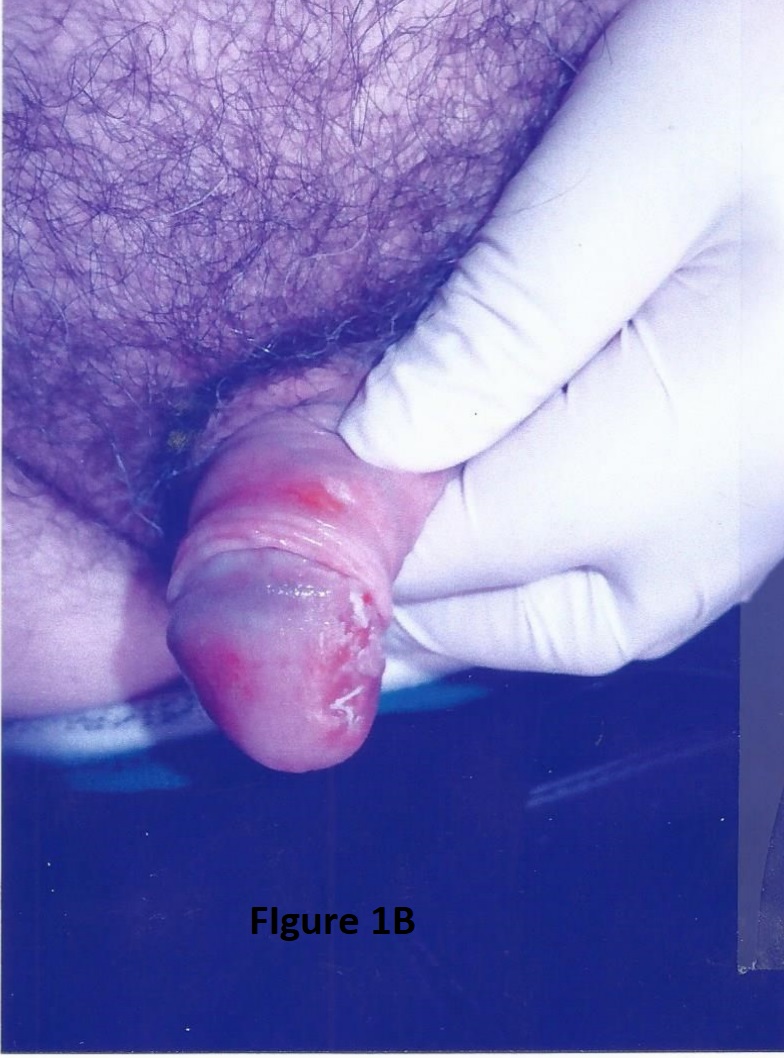
By February 2017, 11 months after a change of treatment, he returned complaining of urethral burning for one day and a new lesion on the glans penis that had grown over a 10 day period. He denied sexual intercourse. He had received Genvoya for 44 weeks. His CD4 count had increased to 671 and HIV viral load was < 20 copies/mL. Clinical examination revealed a 7 mm raised, whitish, nontender plaque on the glans penis without drainage or lymphadenopathy. (Figure 1A) Treatment included Rocephin 250 mg IM as one injection and doxycycline 100 mg p.o. b.i.d. for 21 days under the presumption that he might have gonorrhea, chlamydia, or chancroid. Viral cultures and CBC, CMP, RPR, Chlamydia, Bartonella titers, and urinalysis came back as unremarkable, except for an RPR of 1:1.
Two weeks later, the penile lesion remained unchanged. The patient reported 7/10 constant pain. He began treatment with Bicillin 2.4 million units IM for three weeks to treat possible underlying syphilis. As the lesion did not improve the following weeks, complete surgical resection was performed (Figure 1B).
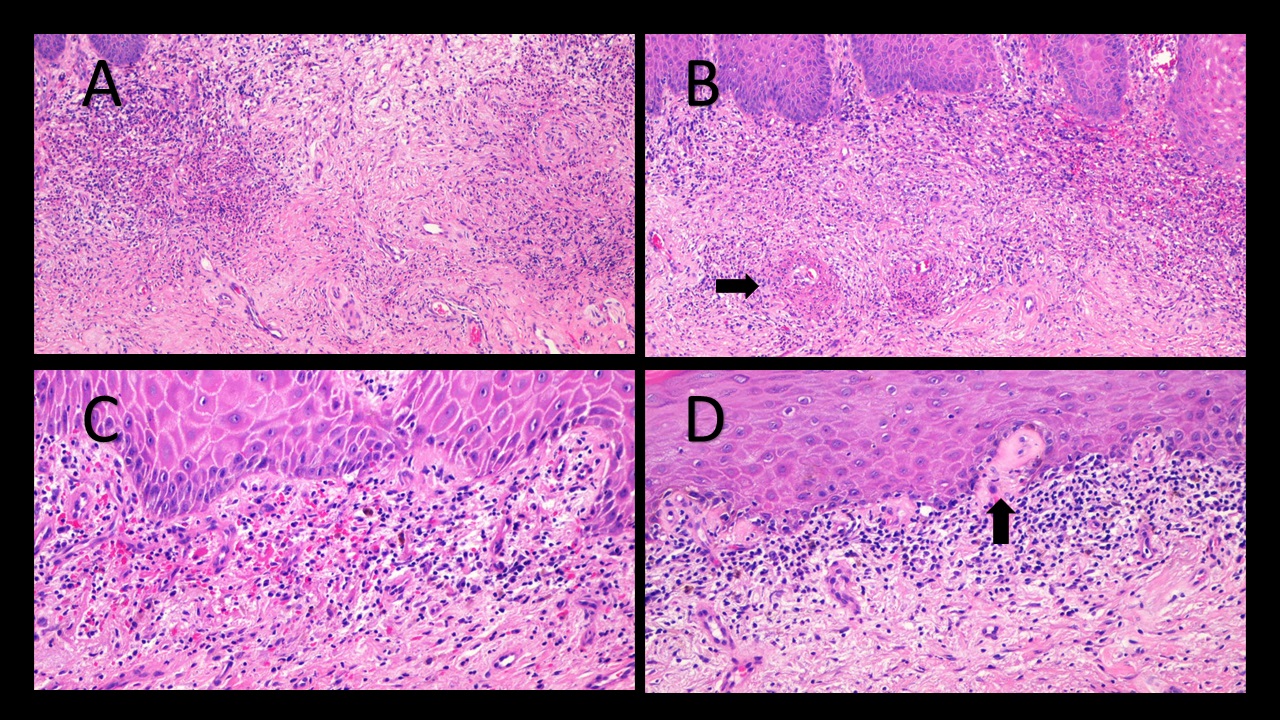
Histologic examination of the lesion revealed epidermal hyperplasia, underlying diffuse dermal fibrosis, and an associated inflammatory infiltrate composed of neutrophils, plasma cells and rare eosinophils in the superficial dermis. In addition, there was fibrin deposition in the wall of some superficial capillaries of the dermis and perivascular neutrophilic nuclear debris as well as extravasation of red blood cells, consistent with leukocytoclastic vasculitis. In addition, there were histologic changes of balanitis xerotica obliterans characterized by a bandlike lymphoplasmacytic infiltrate along the dermal-epidermal junction and deposition of hyaline material in the superficial papillary dermis. Although the overall histologic findings were suspicious for an infection process, AFB, Gomori MethenamineSilver (GMS), Gram, and Warthin-Starry stains were negative for microorganisms. Immunohistochemical studies performed at the Centers for Disease Control and Prevention (CDC) did not show any evidence of spirochetes, including Treponema spp (supplemental).
By March 2017, his penile glans showed complete healing and RPR became negative. As of January 2019, the patient has had no recurrence of the penile lesion. He continued on Genvoya daily and reported no significant side effects. HIV viral load remained less than 20 copies/mL and CD4 count has risen to 706.
Discussion
Advances in new antiretroviral treatments have significantly improved the lifespan and quality of life of patients with HIV infection. As HIV patients live longer, it can be expected that the incidence of atypical clinical presentation of common and uncommon medical conditions would increase in this population due to their altered immune system. Our patient with a long history of HIV infection and serologic finding of possible syphilis represented such a scenario as he presented with a plaquelike lesion of the glans penis that did not respond to the usual antibiotic treatments. Although the clinical history was highly suspicious for an infectious process, the histologic examination of the resected lesion revealed merely diffuse fibroplasia of the dermis and leukocytoclastic vasculitis. Even though there were many plasma cells in the inflammatory infiltrate suggestive of syphilis infection, all histochemical and immunohistochemical studies were negative for microorganisms. As the glans penis also demonstrated histologic changes of balanitis xerotica obliterans (BXO), the plasma cells were deemed to represent a cellular component of the lymphoplasmacytic infiltrate of the concomitant BXO.
From a diagnostic and therapeutic standpoint, it was imperative to exclude the possibility that the patient had secondary syphilis involving the glans penis. It should be kept in mind that leukocytoclastic vasculitis can occur in syphilis patients. However, this is a very rare clinical presentation as a search of the PubMed database revealed only 5 cases of LCV in syphilis patients [5-9] (Table 1A). Most patients presented with the clinical manifestation of systemic leukocytoclastic vasculitis with macules, purpura, or petechiae on the trunk and extremities. There was only a single case with a relatively localized presentation as multiple painless erythematous, eroded papules of the glans penis. The finding of LCV in only males with syphilis intrigues us but we have no clear explanation. In all these cases, LCV was considered as non-specific vasculitis developed secondary to syphilis because of the clinical treatment of syphilis with antibiotic cause the resolution of the cutaneous vasculitis within weeks. Therefore, the penile lesion in our patient was most likely not secondary syphilis despite RPR 1:1 because it presented as a single localized lesion as opposed to extensive dermal involvement. A previously reported case of syphilis presenting as LCV on the glans penis was also associated with the development of erythematous macules on the scalp and palms and positive serologic testing for syphilis at follow-up [7]. In contrast, our patient never developed clinical signs of secondary syphilis and his RPR was negative at follow-up. Reported cases of syphilis associated LCV were effectively treated with Penicillin G, making it unlikely that the lesion in our patient was related to syphilis rather than an immune-mediated process as treatment with Penicillin was unsuccessful and surgical resection provided a cure. (Table 1A) Furthermore, the absence of Treponema on extensive immunohistochemical testing supports an etiology other than syphilis.
As underlying syphilis was ruled out based on the clinical presentation in conjunction with the negative immunohistochemical results for Treponema, and other infectious processes were not likely in the absence of any microorganisms in the histochemical stains, the morphologic findings of the glans penis lesion were deemed to be compatible with EED / localized chronic fibrosing vasculitis. Erythema elevatum diutinum (EED) is a rare cutaneous dermatosis commonly presenting as persistently red, violaceous and yellow papules, plaques, and nodules that are usually distributed symmetrically on the extensor surfaces of the extremities, including the buttocks [1]. An association of EED with a spectrum of conditions, including HIV infection, has been reported in the literature. Of note, reports of atypical clinical presentation such as an isolated lesion, unusual location, or lack of typical associated clinical conditions have been documented in the literature. Carlson and LeBoit coined the term "localized chronic fibrosing vasculitis" for these cases [4]. Penile involvement by EED is very rare. Including the current case, our literature analysis revealed only 7 well-documented reports [10-15] (Table 1B). All cases occur in elderly men (mean: 65.3 years old; range 55 – 74 years). Interestingly, the glans penis is the main part of the penis that is involved in all reported cases with only one patient had additional lesions on the foreskin and penile shaft [14]. Clinically, EED of the glans penis presented as verruciform nodules [10], indurated plaque/mass [11,13,15], or local ulcer [12,14]. Notably, patients with EED involving the glans penis usually presented with an atypical clinical presentation as the penile involvement is the sole manifestation of EED in almost 60% of the cases without any additional lesions in other parts of the body
A recent literature review on EED identified 21 HIV patients among the 133 EED cases for an incidence of 16% [1]. Even though EED has emerged as a possible new specific HIV associated dermatosis, none of the HIV patients to date have displayed EED on the glans penis. Hence, the current case is the first report of an HIV patient with EDD involving the glans penis and therefore broadens the spectrum of EED in the HIV population. Because of the paucity of the literature on EED involving the glans penis, the atypical manifestation of such lesion on the penis, particularly in an HIV patient, could potentially pose significant diagnostic difficulties, in particular in the absence of additional EED lesions in the typical anatomic distribution outside the penis (in 2/3 of the cases as stated above).
Pathophysiologically, EED is believed to involve the deposition of immune complexes in small blood vessels, which leads to an inflammatory response and recruitment of leukocytes. Interestingly, our patient developed the penile lesion 11 months after the change of his antiretroviral treatment that resulted in an improvement in his immune system evidenced by the increase of his T-cell count in the blood and a reduction of the viral load. Because of the seemingly temporal relationship between the presentation of the lesion on the glans penis and the changes of antiretroviral treatment, we hypothesized that the EED on the glans penis may represent a form of immune reconstitution inflammatory syndrome (IRIS). IRIS has been reported to be mediated by both infectious and noninfectious processes in HIV positive patients. Common infectious presentations found in a cohort of HIV-infected adults after initiating antiretroviral therapy include Candidiasis, Cytomegalovirus, and Pneumocystis pneumonia in a cohort of HIV-infected adults as reported by Novak et. al [17]. Our patient had neither the clinical presentation nor serology to strongly indicate an infectious process. In one case of IRIS presenting as a vasculitis, authors felt they could not exclude the possibility that it was directed to HIV-infected endothelial cells [16]. In the absence of a detected infectious process in our patient and the complete resolution of the single lesion following resection, we hypothesize the EED in our patient is immune rather than infectious mediated.
Conclusion
In summary, we report the first case of EED involving the glans penis of an HIV patient which expands the spectrum of EED manifestation in the HIV population. The seemingly temporal association between the lesion on the penis glans and the change of the patient's antiretroviral regimen raised the possibility of an atypical presentation of immune reconstitution inflammatory syndrome. Since EED involving the glans penis is a very infrequent occurrence, particularly in HIV patients, clinicians should be aware of this phenomenon as complete resolution of symptoms following surgical resection in the current patient suggests a potential therapeutic approach for patients presenting with similar lesions.
Acknowledgments
The authors would like to acknowledge Dr. John Andrew Carlson in Albany Medical Center for reviewing the histologic slides.
- Doktor V, Hadi A, Hadi A, Phelps R, Goodheart H (2019) Erythema elevatum diutinum: a case report and review of the literature. Int J Dermatol 58: 408-415.
- Muratori S, Carrera C, Gorani A, Alessi E (1999) Erythema elevatum diutinum and HIV infection: a report of five cases. Br J Dermatol 141: 335.
- Dronda F, González-López A, Lecona M, Barros C (1996) Erythema elevatum diutinum in human immunodeficiency virus-infected patients--report of a case and review of the literature. Clin Exp Dermatol 21: 222.
- Carlson JA, LeBoit PE (1997) Localized chronic fibrosing vasculitis of the skin: an inflammatory reaction that occurs in settings other than erythema elevatum diutinum and granuloma faciale. Am J Surg Pathol 21: 698-705.
- Cam H, Taytan Y, Aji DY, Bilgi Z, Aydemir E, Demirkesen C (2004) Congenital syphilis presenting with nephrotic syndrome and leucocytoclastic vasculitis. J Eur Acad Dermatol Venereol 18: 484-486.
- Chao YC, Chen CH, Chen YK, & Chou CT (2006) A large ulcer and cutaneous small-vessel vasculitis associated with syphilis infection. Scand J Rheumatol 35: 147-151.
- Kim DH, Choi SR, Lee KR, & Yoon MS (2010) Syphilis showing leukocytoclastic vasculitis. J Cutan Pathol 37: 607-608.
- Furlan FC, Oliveira AP, Yoshioka MC, Enokihara MM, Michalany NS (2010) Leukocytoclastic vasculitis: another condition that mimics syphilis. An Bras Dermatol 85: 676-679.
- Li X, Xia J, Padma M, Ma Z, Tian Y (2019) Cutaneous leukocytoclastic vasculitis as the first manifestation of malignant syphilis coinfected with human immunodeficiency virus. J Cutan Pathol 46: 393-395.
- Mizumoto T, Ohkawara A, Ohnishi O, Aoyagi T, Miura Y (1997) Erythema elevatum diutinum, a variant of cutaneous vasculitis. Hautarzt. 28: 516-527.
- Wahl CE, Bouldin MB, Gibson LE (2005) Erythema elevatum diutinum: clinical, histopathologic, and immunohistochemical characteristics of six patients. Am J Dermatopathol 27: 397-400.
- Yoshii N, Kanekura T, Higashi Y, Oyama K, Azagami K, Kanzaki T (2007) Erythema elevatum diutinum manifesting as a penile ulcer. Clin Exp Dermatol 2: 211-213.
- Ziemer M, Schwede K, Simon JC, Paasch U (2013) Atypical erythema elevatum diutinum or extrafacial granuloma faciale? J Dtsch Dermatol Ges. 11: 178-180.
- Syuto T, Tago O, Kuriyama Y, Ishibuchi T, Sasahira S, et al. (2014) An unusual case of erythema elevatum diutinum with penile and laryngeal manifestations. Eur J Dermatol 24: 96-97.
- Harbjerg JL, Krarup KP (2014) Erythema elevatum diutinum on glans penis is a rare manifestation. Ugeskr Laeger 176.
- Iordache L, Launay O, Bouchaud O, Jeantils V, Goujard C, Boue F (2014) Autoimmune diseases in HIV-infected patients: 52 cases and literature review. Autoimmun Rev 13: 850-857.
- Novak RM, Richardson JT, Buchacz K, Chmiel JS, Durham MD, et al. (2012) Immune reconstitution inflammatory syndrome: incidence and implications for mortality. Aids 26: 721-730.
- (2019) Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America.
- Ratnam I, Chiu C, Kandala NB, & Easterbrook PJ (2006) Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis 42: 418-427.


Tables at a glance