Adult Midgut Malrotation: A Case Report
Received Date: July 03, 2020 Accepted Date: July 20, 2020 Published Date: July 21, 2020
doi: 10.17303/jspcr.2020.2.102
Citation:Victor S Alemany MD (2020) Adult Midgut Malrotation: A Case Report. J Surg Proce Case Rep 1:1-5.
Abstract
Background: Midgut volvulus occurs as a complication of intestinal malrotation, a congenital abnormality due to partial or complete failure of normal 270-degree counterclockwise rotation of the midgut around the superior mesenteric vessels in fetal life. Epidemiologically, the incidence of malrotation is about 1 in 6000 live births, with most presenting in infancy. Presentation in adults is rare; a high index of suspicion is necessary to diagnose this condition in adults.
Case Report: A 31-year old male presented to the ED with complaints of a one-year history of intermittent lower back pain with occasional nausea but denied associated vomiting. He stated intermittent diarrhea and denied obstipation. Vitals, basic metabolic panel, and complete blood count were within normal limits. Physical exam was significant only for flank tenderness. CT with the contrast of abdomen and pelvis showed non-obstructed bowel, small intestine to the right of the abdominal midline, and large intestine to the left. Axial imaging was significant for clockwise rotation of mesentery around the superior mesenteric artery and intestine, suggestive of the whirlpool sign; no retroperitoneal duodenum was noted. The patient was subsequently planned for an exploratory laparotomy and Ladd Procedure within 48 hours after diagnosis.
Conclusion:Though most common in infancy, symptomatic midgut malrotation may present in adulthood with non-specific symptoms such as flank pain and nausea due to intermittent volvulus. Imaging is an important modality in diagnosis as well as a high level of suspicion, particularly in the case of adults with the non-acute abdomen, to establish the diagnosis of malrotation and volvulus.
Keywords: malrotation; midgut malrotation; intestinal malrotation; congenital malformation
Background
Midgut volvulus occurs as a complication of intestinal malrotation. Intestinal Malrotation is a congenital anomaly due to partial or complete failure of the 270 degrees counterclockwise rotation of the midgut around the superior mesenteric vessels in fetal life [1]. The narrow-based mesentery twists around itself and also twists around the superior mesenteric artery which increases the risk for ischemic necrosis of the bowel.
The incidence of symptomatic malrotation is about 1 in 6000 live births [2] with many presenting in infancy. Recent studies suggest that about 70 percent present by age 1; other studies have suggested 75 percent of patients present by age 5 [3,4]. Malrotation has traditionally been considered a differential diagnosis more prevalent in the pediatric population. However, some studies suggest, although rare, malrotation may be more common in adulthood than previously considered [5-9].
Due to the lower degree of suspicion, diagnosis in the adult population may be significantly delayed, which may increase morbidity and mortality [9,10]. Time to operation is an important consideration to preserve the viability of the intestine. Failure to recognize midgut volvulus is associated with significant morbidity and may lead to subsequent small intestine resection and possible short bowel syndrome due to ischemic necrosis of the bowel [1].
Initial presentation is most common in infancy and presents with bilious vomiting and failure to thrive. Compared to the pediatric patients, the presentation in adults is more likely chronic with non-specific symptoms, such as intermittent vomiting, abdominal pain, diarrhea, weight loss; these symptoms can be attributed to more common etiologies such as irritable bowel syndrome, peptic ulcer disease, or psychiatric causes [5,7,8].
A high index of suspicion is often necessary to diagnose this condition in adults. In fact, the initial correct diagnosis in the pediatric population is significantly higher than that for the adult population, with a significant delay in diagnosis in the order of months, only because this is not a common presentation in the disease process in adults.7 For those that are found to have malrotation, a Ladd procedure is performed, as in the pediatric population, to reduce the potential for future complications [6,9] Here, we present a case of a 31-year old male with malrotation treated with subsequent Ladd procedure.
Case Presentation
A 31-year old male presented with complaints of a one-year history intermittent lower back pain. He stated that he suffered occasional nausea but denied associated vomiting. He claimed intermittent diarrhea but denied obstipation. The patient had no other past medical history, no previous surgeries, and an unremarkable social history. Vitals were normal and stable and included a blood pressure: 117/66 mmHg, heart rate 57 bpm, the temperature at 98.3° F, respiratory rate 18 rpm, and an O2 saturation 100% on room air. On physical exam, the patient had only left flank tenderness to deep palpation, the abdomen was not distended and didn't present signs of peritonitis.
Basic metabolic panel and complete blood count were all within normal limits. The patient was administered gastrografin for abdominal and pelvic computer tomography (CT) scan as a part of the workup for nephrolithiasis, which was the leading differential diagnosis at the time of presentation. The CT scan revealed a non-obstructed bowel with complete follow-through of the contrast. The small intestine was noted to be to the right of the abdominal midline and the large intestine was noted to be to the left of the abdominal midline as seen in (figure 1).
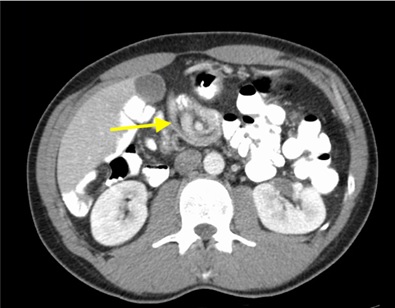
Axial imaging was significant for clockwise rotation of mesentery around the superior mesenteric artery (SMA) with an intestinal whirlpool sign and the absence of a retroperitoneal duodenum (figure 2). The patient was admitted with the diagnosis of midgut malrotation with volvulus. The patient was subsequently taken for an exploratory laparotomy and Ladd Procedure. Postoperatively, the patient recovered quite well and was discharged after post operative day 3. In follow up clinic visits he showed no signs of his initial presenting symptoms.
Discussion
Normal embryological rotation of the intestine starts at 6-week gestation. The intestines overgrow the size of the abdomen. This leads to a normal physiologic herniation of the bowel contents through the umbilicus, associated with a 90-degree counterclockwise rotation around the axis of the superior mesenteric artery. As the fetus continues to grow, the intestine returns to the abdomen at 8 to 10 weeks gestation, which is associated with an additional 180-degree counterclockwise rotation. This makes the total 270-degree rotation of the midgut about the SMA. The cecum subsequently gets attached to the right lateral abdominal wall, retroperitoneally. This rotation sequence leads to a wide base mesentery
Midgut malrotation is considered any abnormality in the normal 270-degree counterclockwise rotation about the SMA. Nonrotation of duodenojejunal limb, followed by normal rotation and fixation of the cecocolic limb, results in duodenal obstruction by abnormal mesenteric bands, the Ladd bands, that extend from the colon across the anterior duodenum. This leads to a narrow-based mesentery, predisposing the patient to volvulus.
For our patient, the CT of the abdomen and pelvis was significant for whirlpool sign, which as stated previously is defined as the twisting of the intestine around the superior mesenteric artery, and duodenojejunal junction positioned to the right of the abdominal midline with cecum to the left of the midline. These findings correlated with our intraoperative findings. The midgut was seen to volvulize but no ischemic bowel was noted. In adulthood, most patients with malrotation present with chronic, intermittent symptoms as in our patient. It is likely these symptoms are due to obstruction from Ladd bands and/or intermittent volvulus. In fact, in our patient, he presented with a oneyear history of intermittent lower back pain that significantly affected his quality of life. The chronicity of his symptoms without diagnosis is common in the adult population even though it is a rare and considered a reportable case in this population [7,8]. The Ladd procedure, first described by Dr. William Ladd in 1936, has been the established surgery for the treatment of malrotation, particularly in children. The same procedure has been utilized in adults with success as in our procedure. The area of the controversy lies in whether or not asymptomatic adults require the procedure [6-8]. Ultimately, the decision to operate must involve an informed discussion between the surgeon and the patient, but if the diagnosis is made by CT scan and the patient has had prolonged symptoms albeit intermittent as in our course, we strongly recommend surgery [8] Most patients treated with the Ladd procedure do not have a recurrence of volvulus. The most common complication subsequent to the procedure is small bowel obstruction due to adhesions, with most patients presenting within one year of operation [2]. Thus, it is important to follow these patients for new presenting abdominal symptoms that may necessitate a return to the operating room.
In the postoperative period, our patient was seen to be doing well with the resolution of his persistent lower back pain. Given the clinical picture with subsequent resolution of symptoms post-operatively, it is likely the patient experienced recurrent midgut volvulus causing his intermittent back pain, which was corrected by the exploratory laparotomy and the Ladd Procedure.
Adult patients with midgut malrotation may present with non-specific symptoms as in our case; the differential may be broad, and a high level of suspicion is needed to make the diagnosis. We argue that malrotation should not be considered primarily a pediatric condition, as malrotation can present well into adulthood, with some cases reported in patients in their 80s and others found incidentally at autopsy [5-8]. Imaging is important in these circumstances to delineate appropriate subsequent management. The whirlpool sign, twisting of the intestines around the SMA, may be suggestive of malrotation and may be found on CT imaging with contrast and/or ultrasound [2].
Conclusion
Although traditionally considered a pediatric entity, symptomatic midgut malrotation may present in adulthood with nonspecific symptoms such as flank pain and nausea. Imaging and a high level of suspicion are needed to diagnose this entity, especially in adults with the non-acute abdomen, as in our patient. The authors argue that it has been since 2018 that an isolated case of midgut volvulus in an adult has been reported, [11] and the case is so unusual, general surgeons need to be aware of its possible occurrence, workup, and treatment.
- Sahu S, Raghuvanshi S, Sinha A, Sachan P (2012) Adult intestinal malrotation presenting as midgut volvulus; case report. Journal of Surgical Arts 5: 18-21.
- Biko DM, Anupindi SA, Hanhan S.B, Blinman T, Markowitz RI (2011) Assessment of recurrent abdominal symptoms after Ladd procedure: clinical and radiographic correlation. Journal of Pediatric Surgery 46: 1720–1725.
- Kotze PG, Martins JF, Rocha JG, Freitas CD, Steckert JS, et al. (2011) Ladd procedure for adult intestinal malrotation: Case report. ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) 24: 89-91.
- Aboagye J, Goldstein SD, Salazar JH, Papandria D, Okoye MT, et al. (2014) Age at a presentation of common pediatric surgical conditions: Reexamining dogma. Journal of Pediatric Surgery 49: 995–999.
- Gamblin TC, Stephens RE, Johnson RK, Rothwell M (2003) Adult malrotation: a case report and review of the literature. Current Surgery 60: 517–520.
- Moldrem AW, Papaconstantinou H, Broker H, Megison S, Jeyarajah DR (2008) Late Presentation of Intestinal Malrotation: An Argument for Elective Repair. World Journal of Surgery 32: 1426–1431.
- Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM (2008) Age-Related Differences in Diagnosis and Morbidity of Intestinal Malrotation. Journal of the American College of Surgeons 206: 658–663.
- Kapfer SA, Rappold JF (2004) Intestinal malrotation— not just the pediatric surgeon’s problem. Journal of the American College of Surgeons 199: 628–635.
- Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM (2008) Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg 206: 658-663.
- Coe TM, Chang DC, Sicklick JK (2015) Small bowel volvulus in the adult populace of the United States: results from a population-based study. Am J Surg 210: 201-210.
- Bhatia S, Jain S, Singh CB, Bains L, Kaushik R, et al. (2018) Malrotation of the Gut in Adults: An Often Forgotten Entity. Cureus 10: e2313.


Figures at a glance