A Historic Case Report of Idiopathic Gingival Fibromatosis In Childhood and Its Management
Received Date: May 21, 2020 Accepted Date:June 17, 2020 Published Date: June 19, 2020
doi: 10.17303/jdoh.2020.7.102
Citation:Houda Chafai (2020) A Historic Case Report of Idiopathic Gingival Fibromatosis In Childhood and Its Management. J Dent Oral Health 7: 1-5.
Background
Gingival fibromatosis (GF) is a rare condition characterized by pathological, diffuse or local growth of gingiva. In severe cases functional, periodontal, esthetic and psychological problems may occur [1].
The condition may be related to hereditary factors and occurs as a non-syndromic hereditary gingival fibromatosis (HGF) or as a part of a syndrome. It may also develop in susceptible individuals as a side effect of systemic medications, including the antiseizure, immunosuppressant, or calcium channel blockers [2,3].
Idiopathic enlargement of gingiva, which has no definite cause, is rare and affects only one in 750 000 individuals, and can occur in both genders and in either of the jaws. It is also known as gingivomatosis or fibromatosis [2,4].
The diagnosis is mainly made on the basis of the patient’s history and clinical features, and on histopathological evaluation of affected gingiva. Early diagnosis is important, mostly to exclude oral malignancy [1].
Treatments vary according to the type of overgrowth and the extent of disease progression, thus, scaling of teeth is sufficient in mild cases, while in severe cases surgical intervention is required. Prognosis is precarious and the risk of recurrence exists [1].
This paper presents oral manifestations of a rare case of childhood Idiopathic Gingival Fibromatosis (IGF) along with its surgical management and follow-up outcome.
Case presentation
A 12-year-old femal child reported to the department of ENT, Maxillo-facial, Reconstructive and Plastic Surgery of University Hospital Hassan II, with swollen upper and lower gums, resulting from a consanguineous marriage of 2nd degree and which presents a statural and mental delay.
The patient had no history of seizures, drug intake, fever, weight loss or any other physical or mental disorder. There was no family history of a similar illness
The gingival enlargement was extensive, involving almost all maxillary and mandibular teeth.
History revealed, that this problem was present for the last five years resulting in difficulty with speech and mastication and causing poor aesthetics.
Examination of the oral cavity shows a mass originating at the level of the two arches, filling the oral cavity, the teeth show diastemas and are caught in the hypertrophic process.
No other mucosal anomalies were evident. Oral hygiene was fair with scarce plaque, no calculus or any other inflammatory component.
Haematological investigations including complete blood count, differential leucocyte count, serum iron and folate levels, erythrocyte sedimentation rate were carried out to rule out any systemic involvement and results were within normal limits.
Mantoux and sputum tests were negative for tuberculosis and so was the chest X-ray.
CT of the face revealed a heterogeneous appearance of the maxillae and a voluminous homogeneous and regular gingival thickening pushing the teeth outwards.
Gingivectomy was performed under general anaesthesia. External bevel incision was made to achieve better gingival contour and aesthetics. Electrocautery was used to achieve haemostasis as well as to reshape the gingival tissue. Proper instructions were given to the patient and parents regarding brushing and maintenance of oral hygiene.
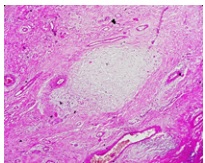
The excised gingival tissue, which was sent for histopathological examination, revealed hyperplastic gingival epithelium covered with stratified squamous epithelium with keratinisation. There was elongation and interlacing of rete ridges. The subepithelium showed extensive fibrosis and focal lymphoplasmacytic inflammation more prominent in the perivascular region There was no evidence of dysplasia or malignancy present. Findings were consistent with idiopathic GF.
A postoperative review after a month revealed complete wound epithelisation. The patient was followed-up at every 3 months. An intraoral examination after 12 months revealed competent lips with good dental occlusion and there was no tendency toward further enlargement.
Discussion
Gingival fibromatosis may occur as an inherited condition known as hereditary gingival fibromatosis, or it may be associated with inflammation, leukemic infiltration, and medications.
The IGF is most commonly associated with hypertrichosis, also occasionally associated with mental retardation and epilepsy. It occurs either as an isolated disease or combined with some rare syndromes like Zimmerman-Laband syndrome (defects of bone, nail, ear, nose and splenomegaly), Murray-Puretic-Drescher.
Gingival hyperplasia in children is less common and is mostly associated with poor oral hygiene and the use of drugs. The granulomatous diseases (Wegener’s granulomatosis, Crohn’s disease, sarcoidosis, tuberculosis), malignancies (acute myeloid leukaemia) and hereditary gingival hyperplasia also should be taken into consideration in the differential diagnosis of gingival overgrowth in children [5, 6].
In the present case, family history was negative. The patient has a mental retardation with no signs of hypertrichosis, and epilepsy or intake of medication known to cause enlargement. Hence, the case was diagnosed as a nonsyndromic case of IGF.
Idiopathic gingival fibromatosis affects the attached gingiva as well as gingival margin and interdental papillae. The cause is unknown, and thus the condition is designated as “idiopathic”. Some cases have a hereditary basis, but the genetic mechanisms involved are not well understood. A study of several families found the mode of inheritance to be autosomal recessive in some cases and autosomal dominant in others [7].
Despite what the name suggests GF is not related to soft tissue fibromatoses that occur elsewhere in the body. Gingiva is typically normal in colour with a firm consistency. It can prog-ress to cover the crowns of teeth and cause retention of primary dentition and tooth impaction. GF often becomes clinically evident with the eruption of primary or permanent teeth, despite the normal appearance of gingival tissue at birth [8].
Histologically, the gingival hyperplasia is mainly due to an increase and thickening of collagen bundles in connective tissue stroma. The nodular appearance can be attributed to the thickened hyperparakeratinized epithelium.
The cellular and molecular mechanisms that lead to this condition are not well understood. HGF keratinocytes seem to have an important role in pathogenesis by inducing extracellular matrix accumulation by fibroblasts [9]. Several authors suggest that more the fibroblasts are present, greater the chance for recurrence [10].
Enlargement usually begins with the eruption of deciduous or permanent dentition; it may rarely present at birth or arise in adulthood. The most extensive enlargement appears to occur during loss of deciduous teeth or in early stages of eruption of permanent teeth. It progresses rapidly during active eruption and decreases with the end of this stage [11].
The management of gingival overgrowth varies according to its aetiology but overall the maintenance of good oral hygiene and periodic surgical excision yield good results. It is recommended that one should wait for repeat surgery until the eruption of all the permanent teeth [12]. Considering the high recurrence rate in cases with GF and the need for repeated surgery, the patient should be kept on regular follow-up.
Studies have demonstrated that recurrence is faster in areas with plaque accumulation [13]. Maintenance of good oral hygiene with professional cleaning and home care maintenance is necessary to prevent the recurrence.
Conclusion
The present case report highlights a nonsyndromic IGF and its management. Surgery significantly improved the patient’s esthetics and masticatory functions. Maintenance of oral hygiene is important to prevent recurrence.
- K.Gawron,K. Łazarz-Bartyzel, J. Potempa,M.Chomyszyn-Gajewska (2016) Gingival fibromatosis: clinical, molecular and therapeutic issues .Orphanet Journal of Rare Diseases 11:9
- Neville D, allen B (2004) periodontal disease. In: Oral and maxillofacial pathology: elsevier saunders.148–50.
- Regezi Ja, sciuba JJ (1999) Connective tissue lesions. In: Oral pathology: clinical pathologic correlations: W.B. saunders :179– 83.
- Ball eL (1941) Case of gingivoma, or elephantiasis of the gingiva. J Periodontol 12:96–100.
- Krishna KB, raju pK, Chitturi rr, et al. (2014) prevalence of gingival enlargement in Karnataka school going children. J Int Oral Health 6:106–10.
- olczak-Kowalczyk D, Krasuska-slawinska e, rokicki D, et al. (2011) Case report: infantile systemic hyalinosis: a dental perspective. Eur Arch Paediatr Dent 12:224–6
- Carranza FA, Hogan EL. (2007) Gingival enlargement. In: Newman MG, Takei HH, Klokkevold PP, Carranza FA, editors. Carranza’s Clinical Periodontology. 10th ed. New Delhi: Elsevier; 373-90.
- Breen GH, addante r, Black CC (2009) early onset of hereditary gingival fibromatosis in a 28-month-old. Pediatr Dent 31:286–8.
- L Meng, et al. (2008) Keratinocytes modify fibroblast metabolism in HGF. Arch Oral Biol 53:1050-57.
- Bittencourt LP, Campos V, Moliterno LF, Ribeiro DP, Sampaoi RK (2000) Hereditary gingival fibromatosis: Review of the literature and a case report. Quintessence Int 31:415-18.
- Fletcher JP (1966) Gingival abnormalities of genetic origin. A preliminary communication with special reference to hereditary generalized gingival fibromatosis. J Dent Res 45:597-612.
- Gawron K,Łazarz-Bartyzel K, Fertala a, et al. (2016) Gingival fibromatosis with significant de novo formation of fibrotic tissue and a high rate of recurrence. Am J Case Rep 17:671–5.
- Mason C, Hopper C (1994) The use of CO2 laser in the treatment of gingival fibromatosis: A case report. Int J Paediatr Dent 4:105-9.


Figures at a glance