Improving Wait Time for Patients Receiving Chemotherapy at Johns Hopkins Aramco Healthcare Oncology Center: A Clinical Practice Quality Improvement Initiative
Received Date: January 19, 2019 Accepted Date: March 06, 2020Published Date: March 09, 2020
doi: 10.17303/jcrto.2020.201
Citation: Dr. Huda Alsayed Ahmed (2020) Improving Wait Time for Patients Receiving Chemotherapy at Johns Hopkins Aramco Healthcare Oncology Center: A Clinical Practice Quality Improvement Initiative. J Cancer Res Therap Oncol 8: 1-8.
Abstract
Introduction: A prolonged waiting time for chemotherapy patients provokes dissatisfaction, insufficient utilization of oncology treatment rooms and compromises patient safety as a result of treatment beyond work hours. Several quality improvement initiatives had been conducted to improve the process at various cancer centers internationally. Resolving issues that contribute to inefficiencies, in conjunction with consistent preparations for next day patient infusion visits, improved cancer patient wait times and patient satisfaction, quality of service and utilization of the Oncology Unit.
Objective: This quality improvement project aimed to reduce the wait time for patients receiving outpatient chemotherapy by 50% over four months, to improve patient satisfaction and increase efficiency at oncology institute in Johns Hopkins Aramco healthcare center (JHAH).
Methods: The action plan was developed and implemented, which included patient assessment through phone triage, performing required lab tests and preparing chemotherapy orders to allow pharmaceutical medication preparation before the appointment date (within 24 hours, or same day before arrival of the patient).
Results: Post action plan data were analyzed and showed a significant reduction in the patient wait times by 60%, from 89 to 36 minutes. This, in turn, reflected an increase in patient satisfaction rate by at least 7% during the study period, nevertheless, the oncology nursing satisfaction rate was also elevated by 23%. In addition to efficient chair utilization at the oncology clinic, while reducing the need for overtime by 51%.
Conclusion: Pre-planning through phone triage nursing assessment, proactively performed lab tests and pre-preparation of chemotherapy has proved to be effective in improving oncology patient wait time as well as better utilization management of treatment rooms. While raising up staff satisfaction and shrinking over time. Certainly, this initiative proved that JHAH is a person-centered hospital as it covered all the STEEEP healthcare quality dimensions.
Keywords: Waiting time; Chemotherapy; Patients satisfaction; Utilization management; STEEEP; Quality dimensions.
Introduction
It is been reported that cancer incidence is increasing dramatically worldwide [1]. The majority of cancer types are treated using different chemotherapy protocols and mostly in repeating cycles [2]. Usually, chemotherapy treatment is administered through an intravenous infusion at the ambulatory oncology centers following well-established policies to ensure chemotherapy prescription quality and administration safety [2,3]. Most chemotherapies need to be prepared at the pharmacy that is a complicated process and takes time. It requires a pharmacist review to ensure a safe and accurate dose. Excessive waiting time for chemotherapy treatment is a common and widely reported problem that cancer patients face at each treatment cycle. This, unfortunately, frustrates both patients and healthcare providers and has been identified as the main cause of overall oncology patient discontent and dissatisfaction [4,5]. Numerous studies had been conducted to look unambiguously at the patient fulfillment impact with respect to waiting time at ambulatory cancer care settings. Long waiting time for chemotherapy had been overwhelming the other aspects of an oncology clinic visit for the patients and families as well [6]. Moreover, the perceived quality of healthcare had been negatively correlated with lengthy waiting times [7]. In addition, this leads to inefficient use of treatment chairs at the oncology unit that in turn result in serving lower patient volume, working beyond working hours to cover the service that will jeopardize patient safety [8].
A quality improvement initiative to reduce the average patient wait time at the National University Cancer Institute- Singapore, has proved that an effective phone triaging composed of pre-preparation of chemotherapy reduced the waiting time significantly by 66% [5]. A similar project at Johns Hopkins Hospital in Baltimore used a multidisciplinary team approach to address wait times. Resolving issues that contribute to inefficiencies, in conjunction with consistent preparations for next day patient infusion visits, improved cancer patient wait times and patient satisfaction, quality of service and utilization of the Oncology Unit (9). Delay could be successfully prevented using quality improvement enterprise and a firm cross-functional team to attain maximal patient's satisfaction [10].
The oncology center at Johns Hopkins Aramco Healthcare Center (JHAH) -Dhahran, Kingdom of Saudi Arabia, deals with a growing number of cancer cases with the increased need for chemotherapy with different protocols, being the mainstay treatment modality for many hematological malignancies and solid tumors. This will intensify the demand for treatment units at the oncology center. A patient satisfaction survey that is published on monthly bases using the “Press Ganey” survey methodology at JHAH revealed that most of the cancer care patients are dissatisfied with the long waiting time at the oncology clinic awaiting to receive their chemotherapy dose. Eventually, this leads to occupying the chairs in treatment rooms, insufficient use of oncology institutes and underserving the patients, thus patient frustration and dissatisfaction. Moreover, receiving chemotherapy after hours of waiting rises the need for nursing staff to work after duty, thereafter staff unhappiness as well. In our study, we aimed to execute a quality improvement project to reduce chemotherapy waiting time by 50% in four months period, and hence elevate the patient's satisfaction. With consideration of preserving the essential inherent safety processes. In addition to increasing the staff gratification and decrease overtime utilization.
Materials and Methods
Ethical approval was obtained from the Institutional Review Board at John Hopkins Aramco Healthcare Center (JHAH) to publish the data and the results of this quality improvement project. Considering this project as a lean 6-sigma project, we followed the DMAIC methodology to accomplish our main goal. (DMAIC is Determine the problem, Measure the baseline, Analyze the current situation, Implement the intervention and Check/control the improvement).
Defining the problem: In this study, we concentrated on chemotherapy patients with nurse appointments but not physician visits. The problem was defined as the cancer patients complained from waiting for a long time in the oncology treatment room until they receive their chemotherapy treatment dose.
Measuring the baseline and analyzing the situation: A process map was performed to look into the details of the cancer patient journey in the oncology center during his/her chemotherapy treatment visit (Figure 1). The operational practice was identified and route cause analysis (RCA) was constructed to determine the major affecting factors drove to the prolonged waiting time (Figure 2).
Pre-implementation data were collected from January to April 2018, to measure the baseline of the current practice, including 8 different chemotherapy protocols, as a sample, for a total of 100 cases. Upon calculation of waiting time during each step in the process, the maximum time was consumed during the preparation of chemotherapy dose. This time duration is starting from releasing the chemotherapy order in the "Epic” system by the nurse, after verifying the protocol and calculating the dose by two pharmacists, up to the complete preparation in the pharmacy preparation room. During this time, patients wait in the treatment room for almost 90 minutes to start their chemotherapy.
Implementation of the action plan: Considering all the possible causes of long chemotherapy waiting time process, and on efforts to close the gaps in the process. A review of articles revealed that international organizations with a similar setting as JHAH have the same concern. They used different approaches that served the same goal in terms of reducing the waiting time to chemotherapy administration. We formed a multidisciplinary team consists of oncologists, oncology nursing, oncology pharmacists, process improvement quality facilitator in addition to oncology management leaders, in order to brainstorm the most appropriate process change that suites the healthcare settings at JHAH oncology institute.
The action plan started in May 2018. The decided action plan that was the more applicable as well as feasible and acceptable by patients at our organization is “pre-planning and proactive work up”. Phone triage approach included calling the cancer patients by the oncology nurse, a day just before the chemotherapy appointment, and perform the required nursing assessment to ensure his/her clinical status, and the readiness to receive the chemotherapy dose. The patient will be asked to do the needed laboratory tests at a nearby JHAH center. Then, the nurse is going to check the result in Epic if the results within normal limits. On the same day, the chemotherapy order in the Epic system would be ready and signed by the oncologist, then as a double safety step, the nurse will review and release the order in the system. Then, the pharmacist verifies the chemotherapy order, checks the correct dose calculation once more and starts preparing the same day or early morning on the appointment day. The chemotherapy will be ready in the unit before the patient checks in at the oncology clinic.
Checking/Controlling the improvement: Post-implementation, data were collected in September for a total of 100 cases, with the same chemotherapy protocols in the baseline data, served during May to August 2018.
Results
Average patients waiting time to chemotherapy administration: Analysis of data showed that we achieved a noteworthy reduction of cancer patients waiting time for chemotherapy from 89.25 minutes to 36.37 minutes, with at least 59.25% improvement. A paired student t-Test revealed a statistical significance with a pvalue of 0.0000023 (considering ≤0.05 as a level of significance) and 95% confidence interval (CI) of 26 to 45 minutes waiting time post action plan (Table 1) (Figure 3).
Oncology Patients Satisfaction Rate: Average patient satisfaction rate for the four months before the intervention was 78%; it was elevated to 84% for the four months after the intervention, with a 6.5% improvement (Figure 4). The “waiting time at Oncology clinic patient satisfaction rate” was significantly affected by the implemented change in the chemotherapy process, as indicated by the patient’s comments and verbatim sayings documented in the “Press Ganey” survey that is sent to patients directly after any visit. This was also confirmed by a personal interview with oncology patients, who received the chemotherapy protocols included in this study, before and after the action plan implementation.
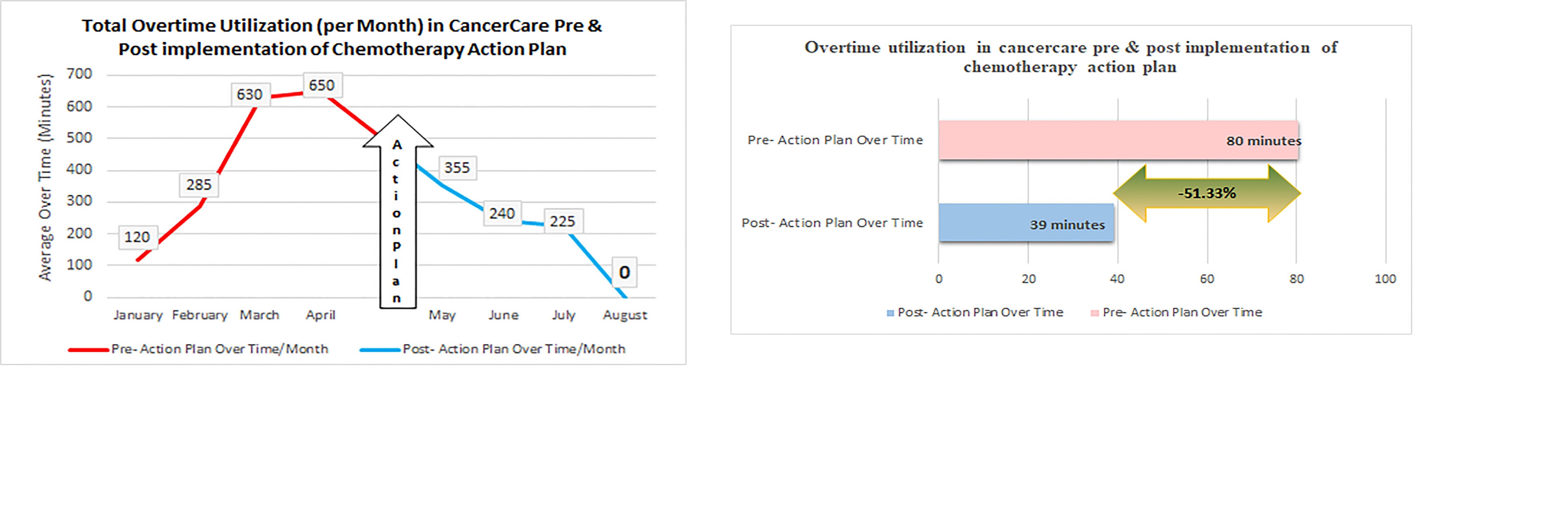
Oncology Overtime Utilization: The implemented change in the chemotherapy process and practice has reflected on underuse of after working hours, as the patient will no longer need to wait for their chemotherapy preparation period. Such practice had declined the overtime by 51.33% post-implementation, which eventually has reduced the cost gradually as shown in the run chart (Figure 5).
Oncology (Nursing) Satisfaction Rate: The oncology nursing staff satisfaction has also affected positively, a questionnaire was given to staff before the implementation of the action plan and the same was filled after the action plan. In summary, overall staff satisfaction was improved by 22.6%.
Sustainability efforts: A data collected after one year of implementing the action plan that is in August 2019. The analysis illustrated further improvement in reducing the waiting time from 36 to 24 minutes (i.e. from 60% to 73% improvement). In addition, the patient satisfaction rate was further elevated to from 84% to 93%.
Discussion
Ultimately, with this quality improvement initiative, we have proved that pre-planning including effective patient phone triage, proactively performed lab tests and pre-preparation of chemotherapy before patient’s arrival, has significantly improved oncology patient waiting time to receive their chemotherapy. In addition, such achievement has led to better utilization of treatment rooms at the oncology center, thus serving more patients. However, this advanced care has influenced patients and staff satisfaction, as well as reducing the overtime utilization and consequently lowering the cost curve.
Certainly, this quality work committed to all the STEEEP healthcare quality dimensions at our organization. We considered patient safety (S) while conducting the change in our practice at the oncology institute. Aiming to reduce the wait timeline (T), using an evidence-based practice that is experienced in other healthcare centers to have an effective (E) change of the practice, managing proper utilization of our resources at oncology to guarantee efficiency (E), ensuring the equity in dealing with all patient levels (E), and finally, it is aimed for patient-centered care (P). Nevertheless, this inventiveness proved that JHAH is a person-centered healthcare center, as we cared about both patient and staff satisfaction.
Absolutely, in order to sustain the change and continue the success, supportive leadership and a firmly structured “Multidisciplinary Team” are necessary. Though, monitoring by steering quality committee and development of KPIs to monitor the performance is very important. Definitely, keeping the ongoing patients engagement surveys for feedback on the healthcare process is of high prominence to persist the advanced care and goodwill.
Conclusion
The overall aim of this quality improvement initiative was perfectly achieved with a precious impact on the reduction of patient wait time for chemotherapy treatment, also on both patient and staff satisfaction level. No doubt, shared vision, supportive leadership, and a fully eager and representative multidisciplinary team were also key.
Acknowledgment: Warmest thanks to our medical staff colleagues at the oncology institute in JHAH who contributed actively to make this quality project successful applying the new plan of change. Thanks to Mr. Ali Abandi from the quality data analytic unit for his help in adjusting the resolution of the images.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA , Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians 68: 394-424.
- Mahrous M, El Shaer E, Rezik L, Taha S,Yosef A (2018) Decreasing prolonged waiting times for chemotherapy administration for patients with cancer. Glob J Qual Saf Healthc 1:44-48.
- Peng Soh TI, Tan YS, Hairom Z, Ibrahim M, Yao Y, Peng Wong Y, Woon Lim S, Eng Lim S, Goh BC, and Tan CS (2015) Improving Wait Times for Elective Chemotherapy Through Pre-Preparation: A Quality-Improvement Project at the National University Cancer Institute of Singapore. Journal of Oncology Practice 11:e89-e94.
- Tan Y. S (2014) Improving waiting time for patients receiving outpatient chemotherapy treatment: a clinical practice improvement project. International Journal of Evidence-Based Healthcare 12:215.
- Kallen MA, Terrell JA, Lewis-Patterson P, and Hwang JP (2012) Improving Wait Time for Chemotherapy in an Outpatient Clinic at a Comprehensive Cancer Center. J Oncol Pract 8: e1–e7.
- Hendershot E, Murphy C, Doyle S, Van-Clieaf J, Lowry J, Honeyford L (2005) Outpatient Chemotherapy Administration: Decreasing Wait Times for Patients and Families. Journal of Pediatric Oncology Nursing 22: 31-37.
- Bleustein C1, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R (2014) Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care 20:393-400.
- Santibáñez P1, Chow VS, French J, Puterman ML, Tyldesley S (2009) Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Manag Sci 12:392–407.
- Collins MB, Szymanski G, Olsen M (2017) Ace in the hole: strategies for the reduction of patient wait times utilizing an interprofessional ambulatory clinical evaluation team (ACE) 2017. Oral presentation at: Oncology Nursing Society 42nd Annual Congress; May 4-7, 2017; Denver, CO.
- Gupta A, Li J, Tawfik B, Pham T, Pathak S, Singh P, Porsa E, Sadeghi N and Li HC (2018) Reducing Wait Time Between Admission and Chemotherapy Initiation. Journal of Oncology Practice; Journal of Oncology Practice 14: e316-e323.

Tables at a glance
Figures at a glance